The Need for Integrated Health Care and Financing Models for Individuals Dually Eligible for Medicare and Medicaid
Objective
RTI worked with the Centers for Medicare & Medicaid Services (CMS) to evaluate two integrated care delivery models, a capitated model and a managed fee-for-service model, under the Financial Alignment Initiative. These models are designed to improve the experience of Medicare-Medicaid beneficiaries and to reduce the fragmentation between the Medicare and Medicaid programs participating in 14 demonstrations in 13 states.
Approach
A mixed-methods approach was used to evaluate the demonstrations’ impact on beneficiaries’ experience, health care quality, service utilization, and costs.
Impact
Evaluation findings and lessons gleaned from the demonstrations’ successes and challenges can inform federal and state policymakers, health systems, consumer advocates, and health plans that are implementing or are considering implementing integrated care models.
In 2020, approximately 12.3 million people were enrolled in both Medicare and Medicaid. Many of these dually eligible beneficiaries, or dual eligibles, have multiple chronic conditions and physical and developmental disabilities. About 40% of dual eligibles have also been diagnosed with at least one mental health condition.
As a result, dually eligible beneficiaries often need:
- Ongoing medical care
- Long-term services and supports
- Prescription drugs
- Behavioral health services
- Supplemental services related to social determinants of health.
Medicare and Medicaid benefits often lack coordination, resulting in fragmented care. In addition, the programs are not well aligned in terms of financing and operational policy. Improving how Medicare and Medicaid integrate care and financing can potentially improve the health of dually eligible beneficiaries and reduce federal and state spending on their care.
The Financial Alignment Initiative’s Role in Improving Health Care for Beneficiaries and Reducing Health Care Costs
In 2011, the Centers for Medicare & Medicaid Services (CMS) launched the Financial Alignment Initiative (FAI) to enhance the quality of care provided to dually eligible beneficiaries, improve population health, and reduce or maintain Medicare and Medicaid spending. The demonstrations aim to develop person-centered care delivery models that integrate medical and behavioral health services and long-term services and supports for Medicare-Medicaid enrollees.
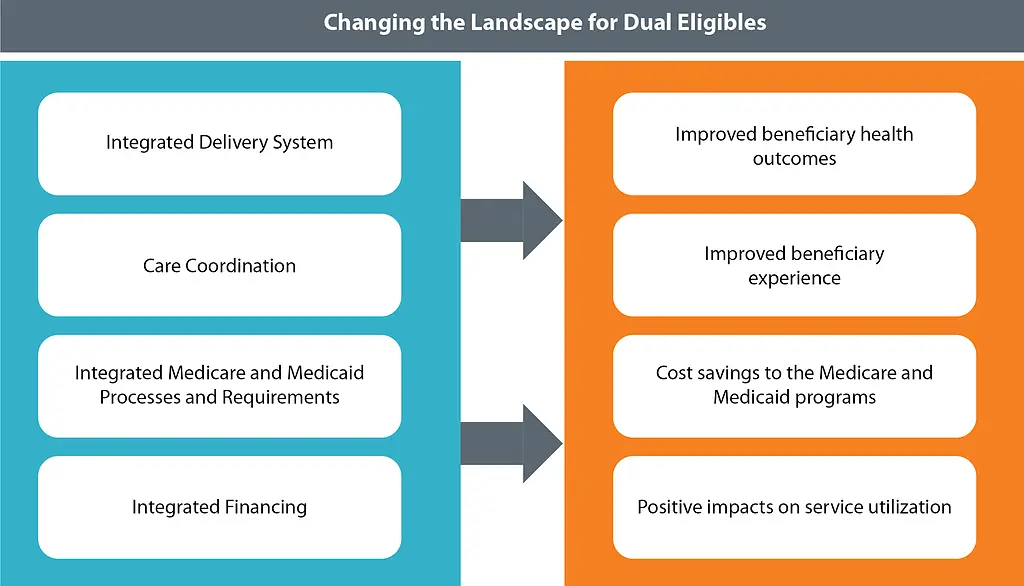
How Do State Demonstrations Under the FAI Work, and How Does This Help Dual Eligibles?
Under the Financial Alignment Initiative, states test one of two integrated care delivery models:
- A capitated model in which health plans coordinate the full range of medical care, long-term services and supports, and behavioral health services.
- A managed fee-for-service model in which states are eligible to benefit financially from Medicare savings that result from Medicaid-covered initiatives to improve quality of care and reduce costs.
Initially, the Financial Alignment Initiative was composed of 14 demonstrations in 13 states. Eleven of the demonstrations employed the capitated model, two implemented the managed fee-for-service model, and one additional alternative administrative model for dual eligibles operated outside of the FAI. Ten FAI state demonstrations continue to date, and many are scheduled to run through 2023. As of December 2020, there were 446,581 dually eligible beneficiaries enrolled in the demonstrations.
Overview of State Demonstrations Participating in Financial Alignment Initiative
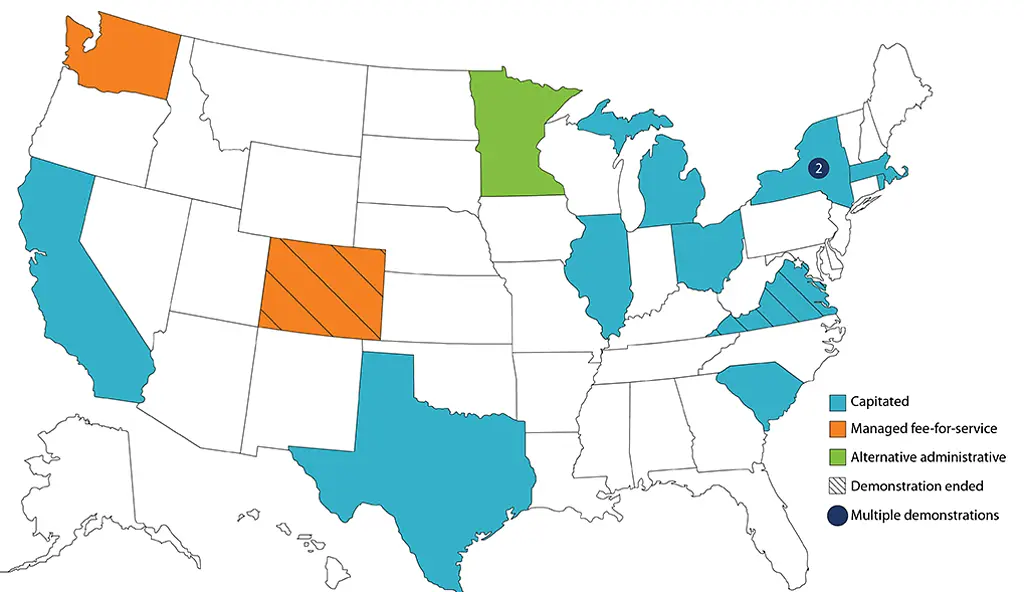
SOURCE: Participating FAI State demonstrations from 2011-present
Evaluating the Demonstrations’ Impact on the Dually Eligible Beneficiary Experience, Health Care Quality, Service Utilization, and Cost
CMS contracted with RTI International to conduct a mixed-methods evaluation of these state demonstrations to:
- Monitor their implementation
- Evaluate their impact on the dually eligible beneficiary experience
- Evaluate their impacts on health care utilization, costs, and quality.
As part of its work supporting the evaluation of the Financial Alignment Initiative, the RTI evaluation team collects information from participating states, stakeholders, and beneficiaries and reviews other relevant studies of beneficiary impact. Our team also analyzes various sources of quantitative data to evaluate the impact on utilization, cost, and quality of care.
The Financial Alignment Initiative evaluation products include individual state-specific reports, issue briefs, and cross-state reports.
What Have We Learned About the Financial Alignment Initiative State Demonstrations?
Our findings show that under the demonstrations, participating states implemented new care coordination approaches, are offering more benefits, and are improving access to social services. Many dually eligible beneficiaries reported improved care coordination and high-quality care and services since enrolling.
To date, RTI’s evaluation also highlighted insights in the following topic areas:
Design and Management
- A contract management team composed of members at the federal and state levels can lead to better design and management in the demonstrations.
- It’s important for state staff on the team to have knowledge of Medicare regulations and policies.
- The stakeholder community should be well-engaged.
Enrollment and Retention
- Eligible beneficiaries are more likely to enroll if they receive easy-to-understand materials in their preferred language.
- Community outreach activities are an important driver of enrollment.
- Timely recertification of the beneficiary’s Medicaid coverage reduces care disruptions and improves the beneficiary’s experience.
- Deeming demonstration eligibility while Medicaid recertifications are processed minimizes enrollment disruptions.
Care Coordination
- Demonstrations seem to have more favorable impacts when they target beneficiaries who are most likely to benefit from care coordination, use person-centered care planning, and focus on care transitions.
- Care coordinators who are trained in patient activation and cultural competence can better engage with beneficiaries, who are in turn more likely to participate in action plans for their own health and in the management of their chronic conditions.
Medicare Service Utilization and Expenditures
- While the demonstrations had a mixed impact on service use, they frequently reduced inpatient admissions and long-term nursing facility placement and increased physician evaluation and management visits.
- Capitated model demonstrations had little impact on Medicare expenditures, while Washington state's managed fee-for-service model significantly reduced Medicare expenditures.
The lessons gleaned from the demonstrations’ successes and challenges can inform federal and state policymakers, health systems, consumer advocates, and health plans that are implementing or are considering to implement integrated care models.
- Centers for Medicare & Medicaid Services (CMS)