Introduction
Brian G. Southwell, Andrea Anderson, Anne Berry, Kamilah Weems, and Lisa Howley
Interpersonal interactions—such as one-on-one conversations between patients and their health-care providers—offer crucial opportunities to mitigate the effects of inaccurate information on patient health and well-being (Abbasi, 2021). Health-care professionals work directly with patients and can discuss pressing personal health concerns and questions with them. Patients in the United States generally continue to trust the health-care professionals with whom they work (Funk et al., 2019). Such trusted relationships can afford spaces in which patients can refer to questionable information that they have encountered, some of which is not consistent with the best available empirical evidence. Clinicians report regular encounters with patients who mention or question misinformation, and yet many clinicians also have not received any formal training for responding to such situations (Wood et al., 2021). That pattern of widespread concern and a paucity of reported training to mitigate the concern suggests the potential for health professions educational curricula to provide explicit tools and tactics for mitigating patient-held misinformation.
As part of a cooperative agreement with the US Centers for Disease Control and Prevention (FAIN: NU50CK000586), the Association of American Medical Colleges (AAMC) launched a strategic initiative in 2022 aimed to increase confidence in COVID-19 vaccines and to address medical misinformation and mistrust through education in health professions contexts. Specifically, the AAMC solicited proposals for competency-based, interprofessional strategies to mitigate health misinformation that operate through new or existing curricula. With this approach, the AAMC staff hoped to help medical schools, along with their nursing or pharmacy school partners, to build their capacity to communicate about health information and dispel misinformation.
Five Health Professions Education Curricular Innovations subgrantees received support from the AAMC to launch their projects in 2022: the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Florida International University Herbert Wertheim College of Medicine, the Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, the Maine Medical Center/Tufts University School of Medicine, and the University of Chicago Pritzker School of Medicine. During a series of meetings over several months, the grantees collectively reflected on the implementation of their ideas and shared their lessons learned. Each team developed a short essay to describe their experience; these essays appear in this report.
We have compiled these insights to inform the practical discussions that many medical educators are currently having to improve their local curricula. We have heard much about the need for health-care professionals to address misinformation held by patients (and by some health-care professionals). Innovative efforts such as those described in the following pages offer some blueprints for concrete steps that medical schools can take to do so.
An Evidence-Based Approach to Helping Patients Who Encounter Misinformation Through Medical, Nursing, and Pharmacy Student Training
Cristina Pelin,*,1 Maya Vasser,*,1 Michael Cassara,1,2 Marie Cavuoto Petrizzo,1 Samara Ginzburg,1 Renee McLeod-Sordjan,1,2 and Joseph Weiner1
1Zucker School of Medicine at Hofstra/Northwell
2Hofstra Northwell School of Nursing and Physician Assistant Studies
*Co-first authors
Background
The emergence of the COVID-19 pandemic and the affiliated “infodemic” led to widespread dissemination of health misinformation across multiple media formats, generating confusion and distrust, with profound global consequences (Lewandowsky et al., 2021). At Northwell Health and the Zucker School of Medicine in New York, a gap analysis revealed that patients expect health-care providers to competently identify health misinformation and feel empowered to address it and that this should be done with attention to cultural/health literacy, equity, autonomy, beneficence, and professionalism.
The current infodemic suggests a new era of public health vulnerability (Lewandowsky et al., 2021). As stewards of our community’s health, we must understand the root causes of this crisis and devise novel curricular strategies to combat it. Our project uses (1) our health system’s extensive experience with COVID-19 and vaccine misinformation, (2) the success of our innovative medical and nursing school programs, (3) our partnerships with St. John’s College of Pharmacy and community-based organizations (CBOs), and (4) our existing teaching Just in Time Teaching (JiTT) application (Ginzburg et al., 2019, and Cassara et al., 2014). We apply these to (1) create a new theory-based model for addressing health misinformation, (2) train our learners to apply this model to address health misinformation with patients, (3) develop novel resources, and (4) apply the model, the training, and the novel resources in real time with patients at a community health fair and receive feedback on the effectiveness of these initiatives.
Project Description
We employed an agile approach to project development and implementation, in which work on both community engagement and curricular threads occurred simultaneously, each informing the other. First, we organized ongoing bimonthly 1–1.5-hour progress meetings. Participants included project leads in curricular development, medical student consultants, stakeholders in the health system that focus on community engagement, faith-based community leaders at a partnering CBO, and liaisons at the pharmacy and nursing schools. In preparation for these meetings, we asked participants to reflect on their previous experience with addressing misinformation, including education or training, encounters with patients and community members, and their perceptions of challenges and associated community needs. During dedicated time in these meetings, we conducted open, unstructured interviews with different stakeholders in attendance. The reflections elicited were documented via interview notes taken in real time.
Second, project leads organized and attended a site visit to our selected partnering CBO as part of planning for a community health fair to address misinformation. Leads met with community volunteers and leaders to reinforce rapport, assess onsite resources available and needed to support a health fair, and engage in health fair logistical planning.
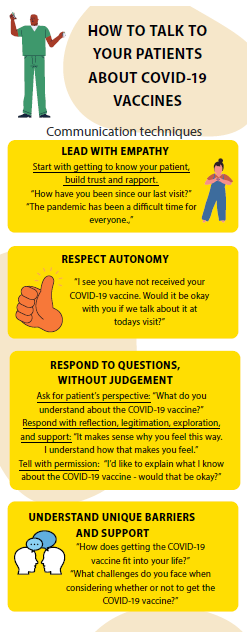
Lastly, we examined the existing curriculum, informed by discussions with both experts in vaccine misinformation and in patient-physician communication. This allowed us to identify opportunities for expansion of curricular activities to acquire knowledge about misinformation and skills to address it. We designed educational tools in the form of sample role plays for use with standardized patients during Objective Structured Clinical Examinations (OSCE) and JiTT infographics (Figure 1) to aid students in real life conversation with patients at the community health fair.
Insights and Lessons Learned
In designing this initiative, we had three expected outcomes:
To build competencies to address misinformation via curricular change.
To apply, assess, and re-practice skills developed through implemented educational sessions.
To strategically impact patient care by equipping our trainees with tools to address misinformation at the interface of direct patient care.
In our planning discussions, we found that most questions elicited the voices and experiences of our students and of patients themselves—the representatives of our goals and those to whom we hold ourselves accountable.
A few key thematic elements arose from this, including the existence of a deep-seated mistrust in health-care systems, predominantly among communities that have historically been disenfranchised, disempowered, and hurt by these same systems, particularly Black, Indigenous, and People of Color communities. This was coupled with lack of comfort among medical students when engaging in conversations about vaccine hesitancy and misinformation, out of fear of confrontation and out of a commitment to rebuild trust effectively, rather than perpetuating past mechanisms of mistrust. Conversations with patients at the health fair primarily related to the COVID-19 booster and included questions about eligibility for, side effects of, and nearby locations to receive the booster; how the COVID-19 vaccine interacts with other vaccines; and whether it is safe to receive multiple vaccines simultaneously.
We found that to effectively partner with the community and engage in cultural humility that work had to come first: our dialog with the community had to drive our educational mission, rather than the other way around. Thus, we sought to engage community leaders through Northwell and the Zucker School of Medicine’s existing CBO partnerships.
In designing our health fair, we found it helpful to discuss, in addition to vaccines and vaccinations, other topics that our participants were seeking information about to engage participants in conversation and to address their current needs. This led to creating a large-scale health fair with the unifying theme of infusing agency and health autonomy back into the community, while empowering patients not only with information but also with the ability to distinguish misinformation from accurate, evidence-based findings. We aimed to achieve this by discussing illnesses prevalent in the community for which community members were seeking information, including high blood pressure, diabetes, the relationship between mental and physical health, and nutrition. Team members involved in this project were experts in diverse fields, including endocrinology, psychiatry, pediatrics, pharmacy, nutrition, and more. We therefore also saw this health fair as an opportunity to leverage our individual skills and areas of expertise toward the collective goal of empowering communities with information.
Discussion with our CBO revealed that these types of efforts are most successful when women and mothers in the community are the primary audience, as they often decide to bring their families to participate. Also, a multidimensional experience that invites discourse and engagement through interactive learning opportunities, appeals to those of all ages, and offers tangible, thoughtfully selected prizes can be more effective than passive learning. Furthermore, having honest and direct conversations is at the core of growing the patient-physician relationship.
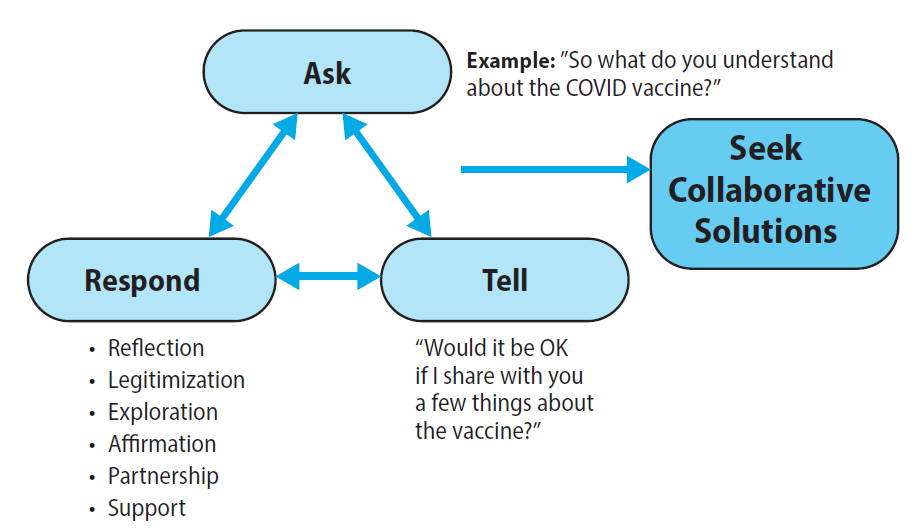
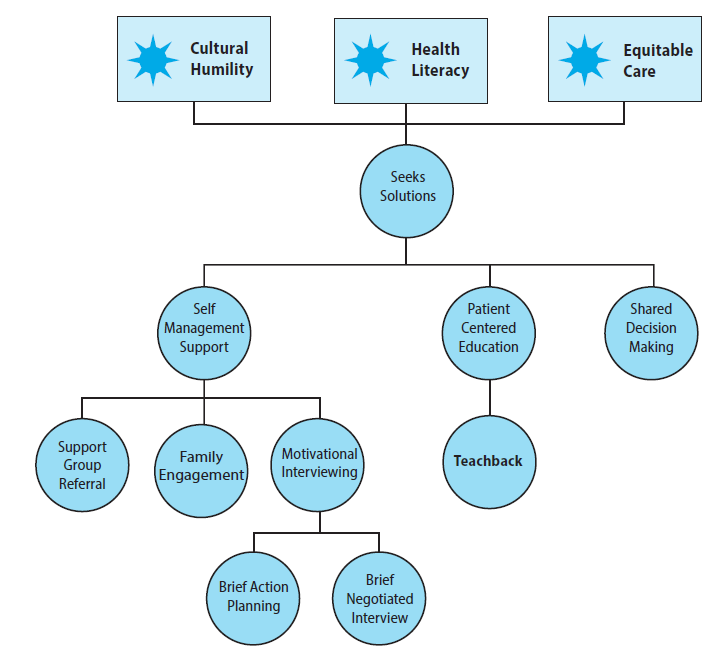
Before the development of our communication skill-building sessions and OSCEs with standardized patients, we took inventory of existing models within the medical school curriculum. Our pedagogical values include active learning, reflective practice (Schon, 1984), and deliberate practice (Ericsson et al., 2018), which promote attainment of enduring competence in learned skills. Additionally, the Ask, Respond, Tell framework (C. M. Chou, 2017), teachback (Schillinger et al., 2003), motivational interviewing (Miller & Rollnick, 2012), and shared decision making (Alston et al., 2014)—which have been shown to be the backbone of collaborative patient physician relationships—are key curricular threads taught to our medical students early in their academic careers (Figures 2a and 2b). These models are dually applicable because they are also fundamental communication strategies for combating vaccine misinformation (Cole et al., 2019).
Our students go through a multistation OSCE approximately every 12 weeks throughout first, second, and third years of the educational program. A set of communication skills are assessed during every OSCE station from our “core communications checklist.” During the first year of medical school, significant variability is observed in student performance in this area. All students get close to “competence” during their second year (except for rare outliers), and by their third year we see, after an initial dip in communication competency most likely due to cognitive overload, the rebound and maintenance of skills. This has taught us that communication skill development, which is critical to addressing misinformation, benefits from spaced learning and an interweaving of concepts and skills assessed.
Although our team consists of clinicians with the professional expertise to engage in conversations about vaccine information and misinformation and to hold these conversations with their own patients, our next steps were to collaborate with experts in communication on vaccine misinformation. Through these discussions, team members identified gaps in the pre-existing curricular activities and uncovered important ways to develop the new sessions. Further, medical student consultants were able to reflect firsthand on the perceived effectiveness of existing curricular sessions. Using both expert content opinion and direct learner experiences has allowed for well-rounded discussions on the creation of the vaccine misinformation curricular content. This has offered us an important insight, emphasizing the need for collaboration with multiple parties, each at different stages in their careers, education, and background. The combination of perspective from clinicians, medical students, communication experts, and community leaders has allowed us to identify our gaps, fill them, and begin to develop innovative lesson plans, OSCEs, and JiTTs.
By first identifying the strengths of our existing curriculum, we were able to adapt these existing models, rather than creating new models, maximizing our time and resources. Further, using logistical practices, such as delegation of roles among team members and bimonthly meetings with agenda setting, has allowed for efficient teamwork and task prioritization.
In summary, the prevalence and perpetuation of misinformation that has occurred in the context of the COVID-19 pandemic has left patients vulnerable. We seek to address these concerns through our ongoing goals of skill-building and conversational competency improvement among practitioners. We hope to highlight the importance of leveraging existing curricular strengths and the value of collaboration between team members, patients, and CBOs.
Addressing Vaccine Misinformation: An Online Motivational Interviewing Module and Telehealth Standardized Patient Exercise to Address Misinformation With COVID-19 Vaccine–Hesitant Individuals
Lexie Morales,1 J. Mark Saunders,1 Emiri Uchiyama,1 Laura Fothergill,1 Deborah Sherman,2 and Rebecca L. Toonkel1
1Florida International University, Herbert Wertheim College of Medicine
2Florida International University, Nicole Wertheim College of Nursing
Background
Despite the efficacy and availability of vaccines against COVID-19, a substantial percentage of the US population remains unvaccinated. Unfortunately, unvaccinated individuals now comprise most of those hospitalized with severe disease (Centers for Disease Control and Prevention, n.d.). Data suggest that many of these individuals are vaccine hesitant but not completely opposed to vaccination (El-Mohandes et al., 2021). Many factors, including the spread of scientific misinformation, may contribute to vaccine hesitancy (Southwell et al., 2022). Misinformation about COVID-19 is abundant, available through various sources, and found in many forms (Simon et al., 2020). To address misinformation about COVID-19 vaccination most effectively without causing unintended consequences (such as defensiveness or blame) for vaccine-hesitant individuals, health-care providers must be able to engage with each individual’s particular concerns regardless of the source of the concern or its basis in fact (Southwell et al., 2019).
The World Health Organization supports the use of motivational interviewing in the general vaccine-hesitant population (Gagneur, 2020), but little is known about its use with COVID-19 vaccine–hesitant individuals (Gabarda & Butterworth, 2021). Preliminary data from the Herbert Wertheim College of Medicine suggest that at least 40 percent of medical students are not confident in their ability to counsel COVID-19 vaccine–hesitant individuals. Though data are not available from other health professions students, similar rates are likely. To address this unmet need, we developed a highly interactive online module that addresses health misinformation by teaching basic motivational interviewing competencies, how to identify vaccine-hesitant individuals, how to use the “Ask-Tell-Ask” model to effectively share information, and how to set SMART (Specific, Measurable, Achievable, Relevant, and Time-Bound) goals to move closer to vaccine acceptance (Epton et al., 2017).
Project Descriptions
In addition to an online module that provides and assesses knowledge necessary to engage meaningfully with vaccine-hesitant individuals, our curriculum also requires learners to engage in a telehealth-style standardized patient encounter in which they must employ the communication and telehealth competencies necessary for optimal health-care delivery in a post-COVID world. After the standardized patient encounter, a structured self-reflection activity reinforces self-directed learning skills. Finally, trained learners are invited as members of interprofessional teams to put their skills to use at organized community-based activities to interact with potentially vaccine-hesitant individuals.
Insights and Lessons Learned
Some challenges faced in the implementation of this program included issues accessing technology, scheduling standardized patient encounters due to the many participating programs, and keeping pace with rapidly evolving information about COVID-19. First, we struggled to develop a version of the online platform that learners could easily access at multiple sittings without having to repeat completed activities. Initial beta tests of the online module revealed that many students preferred to complete it in blocks and therefore lost completed data upon logging out. This problem was solved by developing SCORM (Sharable Content Object Reference Model) versions of the module embedded in each program’s course homepage of the university’s learning management system (Canvas).
Another problem we encountered was implementing standardized patient scheduling while scaling the reach of the program. Although the module was initially offered to medical students, we expanded our reach to include students from other allied health professional programs including the Master in Physician Assistant Studies; Graduate Nursing; Physical Therapy, Occupational Therapy, and Speech and Language Pathology; and the Graduate Certificate in Molecular and Biomedical Sciences programs. Allotting time for students to complete the module and the standardized patient exercise without interfering with their required coursework was initially difficult. To address this issue, a Google document with available standardized patient timeslots was embedded in the online module. This allowed learners to select and reserve a time that worked best for them.
Finally, because of the rapidly changing epidemiology of COVID-19, initial resources developed for community outreach required changes. Student leaders spearheading community outreach efforts found that information regarding risks, treatments, and vaccination recommendations often changed, causing information to be outdated. Rather than printing most materials, we have developed QR codes linked to frequently updated public sites to ensure that information provided is timely.
Several important and generalizable lessons have been learned through the implementation of the program. First, communication between team members is essential. Early and frequent communication with our information technology team helped to fix several technical issues in the roll out of the module. Also, coordination with heads of other allied health schools allowed us to increase the reach of the program and to address scheduling challenges.
A second lesson learned is the importance of flexibility. Although we could not predict every problem that would arise and had extensively planned our online rollout, unforeseen scheduling problems and login issues occurred. The ability to recalibrate quickly as problems developed was critical.
Finally, while our project focuses on COVID-19 vaccine hesitancy, we have learned that the skills taught, and the method employed to teach them, may be used to address vaccine hesitancy more generally. As the pandemic wanes, we hope to use similar methods to address misinformation around vaccine administration in the pediatric population.
Mitigating Medical Misinformation and Mistrust Through Effective Team Communication Using Innovative, Competency-Based Interprofessional Instructional Design
AlisonM.Vargovich,1 NicholasM.Fusco,2 KellyFoltz-Ramos,3 JessicaKruger,4 and WilliamA.Prescott, Jr.2
1University at Buffalo Jacobs School of Medicine and Biomedical Sciences
2University at Buffalo School of Pharmacy and Pharmaceutical Sciences
3University at Buffalo School of Nursing
4University at Buffalo School of Public Health and Health Professions
Background
The World Health Organization named vaccine hesitancy as a top-ten threat to public health in 2019 (World Health Organization, 2019), and the US Surgeon General issued a warning to the American public about the urgent threat of health misinformation in 2021 (Office of the Surgeon General, 2021). In today’s information age, both valid and misleading information about vaccines are readily available on the internet. Social networks can influence perspectives on vaccination (Brunson, 2013; Southwell, 2013), and some individuals misplace trust in professionals outside of health care, those estranged from their medical profession, and nonvetted sources of information (Freed et al., 2011).
Health-care professionals and health professions students will encounter patients and parents who are vaccine hesitant. Trust between patients, families, and health-care professionals; effective communication skills; and an understanding of how to address concerns are keys to improving vaccine acceptance. Health profession students can take an active role addressing vaccine hesitancy and misinformation through community outreach and clinical experiences.
To equip students to influence change, it is important to explain the prevalence of medical misinformation, theory regarding patients’ stages of change (e.g., Prochaska & DiClemente, 1994), and strategies to communicate health information and dispel misinformation. Our goal was to develop a competency-based educational experience for health professions students to develop these skills.
Project Description
Our educational innovation is competency-based, interprofessional, and employs a hybrid instructional design strategy. Competency-based education ensures that students possess the required knowledge, skills, and attitudes at completion. To address misinformation and vaccine hesitancy, we employ evidence-based communication practices informed by the Transtheoretical Model (Miller & Rollnick, 2012) and underlying change factors of self-efficacy, motivation, and interpersonal alliance (Britt et al., 2004), with a clinical focus on motivational interviewing (Gagneur, 2020; Zolezzi et al., 2021) and brief intervention strategies (Leask et al., 2012). These factors and tools support what is needed for belief updating when discussing beliefs formed due to cognitive, social, and affective drivers, as is most often the case for vaccine hesitancy (Ecker et al., 2022).
Our hybrid instructional design strategy includes three components: (1) asynchronous online modules, (2) virtual simulations, and (3) in-person high-fidelity simulations. The asynchronous online learning consists of short, pre-recorded modules summarizing: (1) the infodemic and misinformation surrounding the COVID-19 pandemic, (2) vaccine hesitancy, (3) the value of an interprofessional approach to combating medical misinformation surrounding the COVID-19 pandemic, and (4) evidence-based communication practices informed by the Transtheoretical Model (e.g., motivational interviewing). Students will have access to these modules through our learning management system and will complete them before advancing to the virtual simulations.
We designed two virtual simulation scenarios to allow students to apply knowledge and practice communication strategies introduced in the asynchronous online learning. Students receive feedback in real time and complete guided self-reflection questions. These modules are also available online and are offered to students before their advancement to the in-person high-fidelity simulation.
We designed three in-person, high-fidelity simulation scenarios with standardized actors portraying patients or clients with various levels of willingness to engage in education pertaining to vaccines and the COVID-19 pandemic. The in-person simulation scenarios allow students to implement communication strategies introduced in the asynchronous online learning and reinforced during the virtual simulations. Students work in pairs with a student from a health professions program different from their own and complete all three scenarios, followed by a structured, interprofessional debriefing session where students will receive feedback on their performance.
Insights and Lessons Learned
In developing this activity, we have contemplated our assessment strategy and carefully considered the focus and intention of our outcome measures. Originally, our assessment plan included student self-assessment data, along with standardized actor assessment of student performance for all student participants. We felt these data would be useful in understanding student growth that may or may not have occurred because of participating in the experience. However, these measures do not necessarily give us information on whether our methodology or approach is the optimal way to teach and develop these skills in part because of potential bias in self-report.
After much discussion, we decided to split our cohort into two groups to allow comparison of performance. Students will complete the same self-assessment instrument; however, they will receive the educational materials differently. The first group will receive the online, asynchronous modules and the virtual simulation scenarios at the same time and will be allowed to navigate freely between the two before advancing to the in-person simulation. They have the option of completing the asynchronous, online modules only, the virtual simulation only, or both. The second group will receive the content sequentially: the asynchronous, online modules first, then the virtual simulation, and then advancing to the in-person simulation. The question that we are seeking to answer here is whether there is a benefit to student performance in the in-person simulation with completing the pre-work in a structured, sequential manner as we have traditionally taught in our respective curricula, or whether there is no difference between the two approaches. This, we believe, will better inform us about our pedagogical approach, which in addition to our other assessment data, will be useful for advancing knowledge in this area.
We also can comment on resource investment relative to the project results to date. To develop the educational materials (online modules, virtual simulations, and in-person simulations) the investigators met 1 hour per week during the study period (5 months), for a total of approximately 20 hours. Filming, editing, and publishing the virtual scenarios took approximately 10 hours. Preparing the in-person simulation scenarios, including training the standardized actors, took approximately 8 hours. Hosting the in-person simulation scenarios occurred across two sessions, totaling approximately 6 hours of effort and a monetary expense of $1,800. Therefore, approximately 45–50 hours of faculty effort were spent on this project, and $1,800 were required for 51 students to participate. From the students’ perspective, approximately 2–3 hours are required to complete all three elements of the instructional design.
Moving forward, as the educational materials are more fully developed, faculty effort will be directed mostly toward in-person simulation and debriefing. The monetary cost of using our simulation center is also something that requires a budget; however, there may be opportunities to reduce costs by being strategic with scheduling. For example, adding more standardized actors, and therefore increasing the capacity of students to participate during the same simulation would be more cost effective than scheduling an entirely different session. In sum, the costs of the initial stage of the project are not insignificant; however, the experience has been positive and important for those involved.
Addressing COVID-19 Misinformation in Maine Through Collaborative Learning and Interprofessional Education
Jennifer Hayman,1,2 Shelley Cohen Konrad,3 Linda Chaudron,1,2 Christine Mallar,1 Grace Price,1 Brendan Prast,1 Julia Safarik,4 and Leah Mallory1
1Maine Medical Center
2Tufts University School of Medicine–Maine Track
3University of New England Center for Excellence in Collaborative Education
4Maine Health Department of Medical Education
Background
Vaccine-specific and general misinformation and disinformation have impeded compliance with preventive measures to slow the spread of COVID-19. Studies on vaccine hesitancy show that approaches that directly refute misperceptions have little impact on shifting attitudes (Nowak et al., 2020; Smith, 2022). Studies evaluating effective communication to allay COVID misinformation support use of real-life examples, emphasizing community benefits as effective strategies (Betsch et al., 2017). Effective communication may include motivational interviewing, which has been successful in fostering health-related changes in nutrition, physical activity, behavioral health, and smoking cessation (Gagneur et al., 2019; Lee et al., 2016). The Centers for Disease Control and Prevention recommends vaccine-related communication be delivered by trusted care teams, community health workers, and community agencies (Nowak et al., 2020).
Modern health-care delivery relies upon interprofessional teams. Promoting interdisciplinary collaboration among physicians, nurses, social workers, and advanced practice providers is essential to deliver effective care. Also critical to promoting individual and public health is how prepared all team members are to deliver consistent information to patients operating under health misinformation (Efua Sackey et al., 2022) and to address colleagues whose ambivalence or distrust of the science interferes with health-care practice (Li et al., 2022) and team cohesion.
Project Description
Having knowledge of mitigation strategies to dispel health and vaccine misinformation and recognizing the importance of having a trained team delivering a unified message to patients, we sought to better understand the experience of interprofessional health-care students in clinical encounters with their communities and families. We hypothesize that real-life examples provide insight into experiential learning opportunities and serve as a basis for developing scripting strategies and other educational materials for practitioners to improve communication with patients and colleagues misinformed about COVID-19. These strategies are likely generalizable to other areas of medical misinformation. Ultimately, we seek to create an online curriculum addressing misinformation when talking to patients or other health-care workers that includes didactic and video exemplars using motivational interviewing and other behaviorally based conversation techniques.
To maximize interprofessional input and strategy, Tufts University School of Medicine–Maine Track partnered with the University of New England’s Center for Excellence in Collaborative Education. Initial steps included: (1) performing a literature review of what is currently known on COVID-19 misinformation; (2) conducting focus groups of interprofessional health-care students from two schools of medicine and health sciences education (allopathic and osteopathic medical, social work, physician assistant, and rehab medicine students); (3) conducting qualitative analysis of focus group transcripts to identify drivers of misinformation and vaccine hesitancy; and (4) comparing identified themes to already published data.
Insights and Lessons Learned
Reviewing the literature and focus group data revealed congruence with vaccine acceptance data from the H1N1 and Ebola pandemics, which demonstrated seven areas of influence: (1) demographic factors, (2) trust in health authorities, (3) safety and efficacy of a new vaccine, (4) personal responsibility and risk perceptions, (5) lack of information or misinformation, (6) accessibility and cost, and (7) mitigation measures taken based on decision to vaccinate (Abba-Aji et al., 2022; Truong et al., 2022). Table 1 outlines ideas that highlight nuances related to these factors raised by health professions students.
Table 1.
152576Themes and descriptions from literature and focus group analysis
Experiential observations from the student focus groups resonated with published literature (Earnshaw & Katz, 2020) and informed educational curriculum and standardized patient encounter scripting. As we construct a curriculum consisting of didactic information on COVID-19 paired with examples of motivational interviewing approaches in the clinical setting, we will incorporate focus group suggestions for strategies to employ and avoid when communicating about misinformation (see Table 2).
Table 2.
152577Overview of communication strategies supported in literature and/or by health professions students’ experiential observations
Notes: CDC = Centers for Disease Control and Prevention; WHO = World Health Organization
In summary, our initial experiences with this project provided an ideal opportunity to understand a broad range of health professions perspectives on health misinformation. By identifying themes emerging from interprofessional focus groups, we identified a range of ideas and specific examples that support previous health misinformation research but also provide more specific and nuanced information that will be useful in developing targeted interprofessional curriculum and standardized patient scenarios.
Based upon the information gained, our team developed an open access, online curriculum including didactic as well as exemplar video interactions and collaboratively sponsored a pandemic misinformation symposium available to a broad range of health-care and community professionals. In the next steps of our work, standardized patient trainers and medical script writers collaborating with physician misinformation content experts will work to improve the authenticity of the actor interactions.
In creating the curricula described here, the importance of interprofessional collaboration—including collaboration between patient-facing staff and those who do not directly interact with patients—cannot be overstated. Together, we intend to address patient misinformation thoughtfully, with humility, and in ways that are respectful of patient experiences.
Training Interprofessional Teams to Improve Scientific Communication and Address Health Misinformation in Chicago Communities Using Social Media
Aashna Sunderrajan,1 Sara Serritella,1 Nicole L. Pierce,1 Olabisi Falana,1 Eve Bloomgarden,2 Shika Jain,3 Lisa Mordell,4 and Vineet Arora1
1University of Chicago
2NorthShore University HealthSystem
3University of Illinois
4Loyola University Chicago
Background
Doctors, nurses, and pharmacists play a key role in providing public education on disease prevention and reducing the spread of misinformation. Nurses, doctors, and pharmacists have been voted the first, second, and fourth most trusted professions in the United States (Saad, 2022), respectively. Because of their access to patients (Choi et al., 2020; Marwitz, 2021) health-care professionals have the opportunity to begin a dialog with their patients and provide critical education to improve patient safety and public health. In fact, during the COVID-19 pandemic, tweets containing personal pleas by health-care professionals were perceived to be more effective in shaping attitudes toward the pandemic and were more likely to be shared when compared with formal tweets by policy officials (Solnick et al., 2021).
Unfortunately, health-care professionals are reluctant to engage in social media publicly because of a fear of retribution from their employer (Way, 2020) or because of concerns of being attacked (Pendergrast et al., 2021). Given the status of health professionals as trusted messengers, it is critical to consider how to empower them to speak up against medical misinformation despite the challenges and risks they may incur (Ioannidis et al., 2017).
With these ideas in mind, the Illinois Medical Professionals Action Collaborative Team (IMPACT, 2022) developed a pilot elective for first-year medical students at the University of Chicago Pritzker School of Medicine entitled, “Improving Scientific Communication and Battling Medical Misinformation.” In this course, students were taught how to apply scientific communication principles to identify and address COVID-19 misinformation, focusing on digital and visual communication skills (W. S. Chou et al., 2018). Students also were tasked with creating infographics—applying techniques taught in the lecture series—that subsequently were published on Twitter, eliciting approximately 30,000 impressions (Arora, 2021).
Building on the success of this program, our goal was to lead the development, implementation, and evaluation of an interdisciplinary curriculum—with leaders from medicine, nursing, and pharmacy—that would amplify health-care professionals’ voices and offer them strategies to disseminate evidence-based information to combat misinformation and medical mistrust in their communities.
Project Description
Over the course of a few months, we adapted our existing curriculum to coach health-care professionals on how to identify what misinformation is, where it is coming from, and to provide evidence to the contrary for their patients and communities. This involved (1) didactic lectures on the importance of addressing misinformation in the clinician-patient relationship, the science of storytelling techniques and strategic communications, and the impact of leveraging a group identity to amplify on social media; as well as (2) workshopping sessions where health-care professionals learned to identify misinformation common in their communities, use evidence-based approaches to address these misconceptions, and then disseminate their work on social media and other platforms.
To cater to the needs of our interprofessional group, we made three key changes from our original curriculum. First, because of the short time frame, we condensed our original curriculum into a 3-week course, placing a heavier emphasis on students’ active learning through workshops. Second, because of our students’ dissimilar work schedules, we pivoted to a fully virtual course, held over the lunch hour. Finally, because we wanted to foster an interprofessional environment, we had students work in groups on their projects, with breakout rooms facilitating collaboration.
Insights and Lessons Learned
Interdisciplinary Collaboration and Curriculum
To develop and implement our curriculum, it was imperative that we had an interdisciplinary team of leaders to plan, administer, and participate in the course. Perhaps because of the prominence of misinformation in the current discourse, we found that collaboration across academic boundaries was welcomed, and we were able to form a team of leaders, including the dean of medical education (Vineet Arora), a science communication expert (Sara Serritella), a nursing manager (Nicole Pierce), and a pharmacy education manager (Olabisi Falana).
An interdisciplinary curriculum is characterized by the interweaving of disciplines to teach a subject from multiple perspectives. In our case, this involved identifying the misinformation prevalent in medicine, nursing, and pharmacy; the unique barriers professionals from these fields may have to addressing misinformation; and the different approaches professionals can take to combat these misperceptions with their patients and communities. For example, each of our groups picked topics that reflected their clinical experience, including a dermatologist who led a project on the importance of sunscreen and a pharmacist who led a project on the safety of over-the-counter medications. Early comments from students in this course recognized the benefits of such a curriculum, emphasizing that learning and retention are enhanced when course content is meaningful and relevant.
Synchronous Versus Asynchronous Methods
To cater to the different demands on our medical, nursing, and pharmacy professionals participating in our curriculum, we relied on a combination of synchronous and asynchronous methods. Zoom sessions provided a classroom experience where students learned from didactic teaching. Breakout rooms then offered interactive spaces for students to engage in real-time, collaborative discussion and learning. Recordings of each lecture, including resources discussed, were then made available on Box for students, including those who were unable to attend the Zoom sessions, to access asynchronously.
Although the asynchronous approach offered flexibility, those who primarily relied on this method missed out on opportunities to learn interactively, by engaging with the lecturers and collaborating with their peers. As people learn most and best retain knowledge through exploration and application of that knowledge, it is likely that those who missed this opportunity did not gain as much out of this curriculum. This can be a drawback of asynchronous methods and requires an exploration of how to make this approach more engaging and interactive.
Future deployment of training also raises issues of scalability and reach. Some readers may be interested in possibilities for measuring reach and engagement for efforts like this; Rotolo et al. (2022) explores reach and engagement measurement for social media efforts like ours.
Professional Differences in Pedagogy
Our curriculum involved a combination of didactic teaching and workshops. The lectures provided students with a foundation on how to improve scientific communication and address misinformation; the workshops provided students an opportunity to become active participants and apply that knowledge in a context with which they were familiar. During this course, however, we found differences in pedagogical preferences based on profession, with some preferring one type of learning over the other. For example, medical students preferred to receive direct didactic information, while those from nursing and pharmacy often preferred to participate in interactive workshops. This led to variable attendance during the sessions.
Although we encouraged students to share their infographics on social media, sharing was ultimately each student’s personal choice, and we found differences in how students decided to share their infographics. For instance, medical students often selected to address myths found in their communities of practice and used Instagram as their dissemination platform. Pharmacy and nursing students, however, often selected to address myths held by their patients, and thus, decided to turn their infographics into fliers that they could directly hand out. Going forward, it will be important to understand what the different pedagogical needs are for each profession, and how best we can meet them in a course such as ours to keep engagement high.
This project shows that it is possible to work collaboratively on the development and implementation of an interdisciplinary curriculum to tackle misinformation with health-care professionals. However, consideration of the aims of the curriculum and the core audience is necessary to determine how to implement the course, including whether to prioritize a flexible or an interactive course and use didactic or workshop components. Overall, though, our experiences show that health professionals have vast interest and need to learn more about addressing misinformation, and thus, continued work in this area is imperative.
Observations Across Projects
Brian G. Southwell, Andrea Anderson, Anne Berry, Kamilah Weems, Lisa Howley
What can we learn from these reflections? Several themes evident in these essays hold practical implications for medical schools and health professions educators considering how to address misinformation through curricular innovation. For example, consider the following:
Interprofessional education is valuable, and yet differentiation and coordination are critical when developing curricular interventions to train a wide range of learners. Students being trained for different types of health professions jobs face different constraints in terms of incentives, scheduling logistics, and even the nature of patient encounters.
Effective integration, timing, and convenience matter. Several project teams acknowledged the importance of recognizing how busy faculty and students are and how much information they face in any given day. Tools that support efficient integration into existing curricula and clinical learning experiences, such as the Hofstra/Northwell team’s Just in Time Teaching Tool, can provide easy-to-digest and useful tips moments before or during a patient encounter.
Using exhaustive fact-checking and direct misinformation correction as a primary strategy for patient engagement can be challenging and may not be as effective as other approaches, especially in situations like that posed by the COVID-19 pandemic, in which available information and empirical evidence shifts quickly. Finding ways to educate patients about the nature of science and discovery and steer patients to credible sources of information that are regularly updated may be as important as providing point-by-point correction of misinformation.
Undoubtedly, misinformation is a salient and pressing focus of concern among health professionals. Programs that train those professionals can provide important support, and yet it is also clear that revising and improving medical school curricula to meet this concern will require patience, consistent effort, and careful planning to encourage long-term patient engagement strategies that the next generations of health-care professionals can systematically adopt and implement.