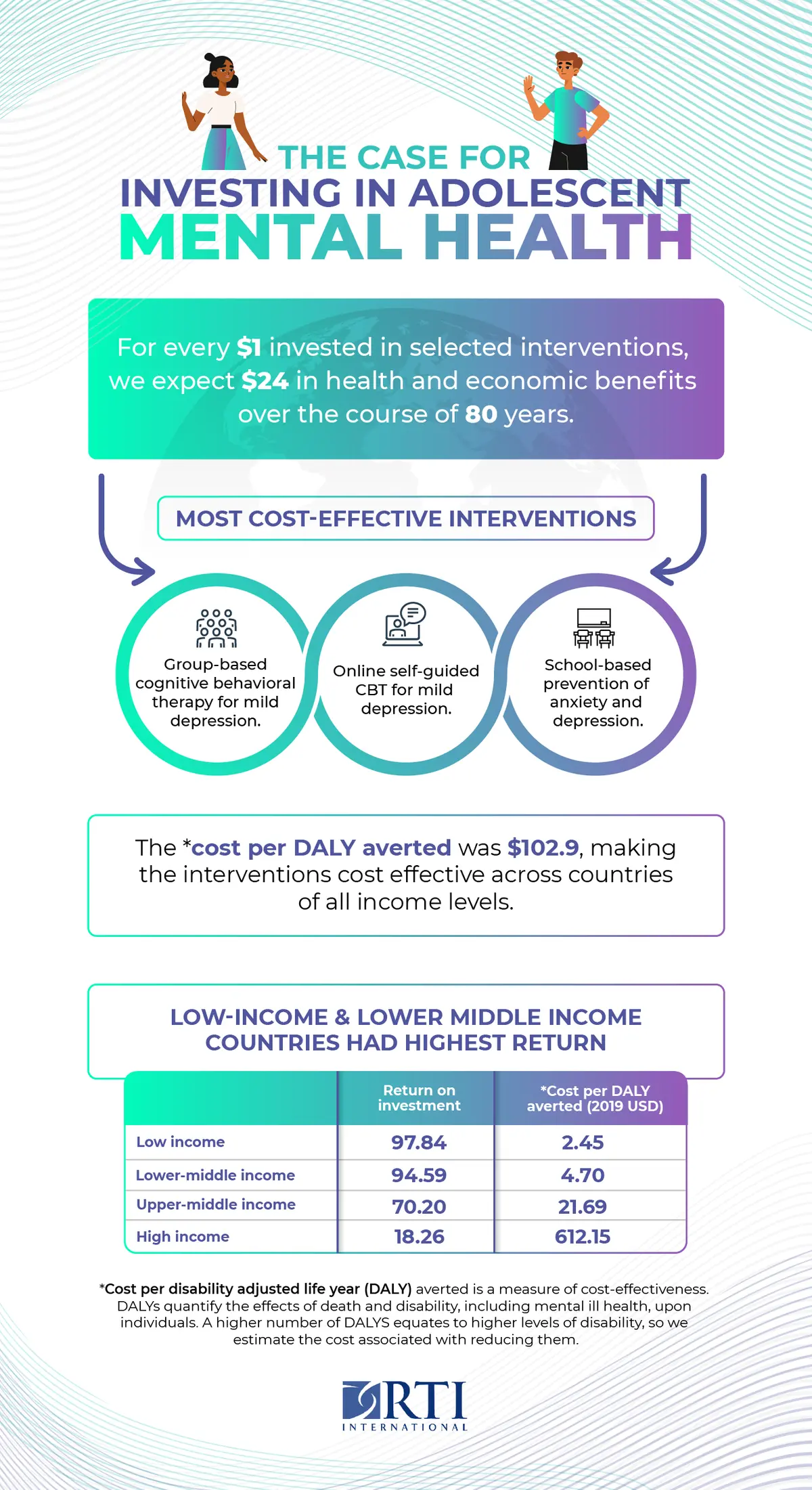
Globally, about 166 million adolescents (ages 10-19) in the world experience mental disorders, but the vast majority (as many as 80%) remain undiagnosed and untreated. Our new global investment case finds that for every $1 invested in the full set of interventions to prevent and treat anxiety, depression, bipolar disorder, and suicide among adolescents, we project $24 in health and economic benefits over the course of 80 years across the 36 countries included in the model.
As recognized in the new World Mental Health Report, a majority of lifetime mental disorders begin to appear in adolescence and young adulthood. In many countries, the COVID-19 pandemic and associated control measures have worsened young people’s mental health. School closures and lockdown measures are associated with increases in severe anxiety and depression and in self-injury and suicide attempts. The pandemic exposed the fragility of adolescents’ mental health and indicated that a multisectoral and systemic response is needed to effectively address adolescent mental health needs.
Adolescent mental health prevention and treatment programs
A number of preventive interventions and treatment services have proven effective in a range of settings, including schools and communities as well as health services. Prevention and treatment remain insufficient in many countries, hence further investment in such effective approaches is key. Our results illustrate that scaling up access to these interventions would have substantial health and economic benefits.
Investment cases illustrate the anticipated impact of health programs and policies by assessing their costs to implement and their health and economic benefits to the population. Understanding the resources required and the expected benefits of introducing or scaling up a program can help policy makers understand the importance of investment and guide their decisions and can assist advocates making the case for that investment.
The return on investment of interventions to protect adolescent mental health
We found that for every $1 investment made in the full set of interventions in our global investment case, we anticipate $24 in benefits over 80 years. This result means that the interventions effectively pay for themselves 24 times over the course of 80 years. These benefits include improved quality of life, increased likelihood of completing education, reduced absenteeism from work, and lower rates of premature mortality among young people now and in later life.
Click here to expand.
Cost-effective approaches to protecting adolescent mental health
Among the interventions included in our analysis, the most cost-effective were those to treat mild depression through group-based cognitive behavioral therapy (CBT) or internet-based CBT. The strong return on investment results for these interventions results from their efficient use of provider time to help multiple adolescents at once as well as the strong link between treating depression and thereby preventing suicide.
School-based programs to prevent anxiety, depression, and suicide also provided high ROIs, indicating that the interventions are cost-effective. These ‘universal’ programs include all young people within an age cohort in a school, regardless of their mental health, and emphasize preventing problems before they arise or become severe. These positive results highlight the potentially important role for schools for improving adolescent mental health. We explored this topic in more detail in the UNICEF State of the World’s Children 2021 report.
Several interventions returned an ROI less than 1, including treatment of bipolar disorder. This result indicates that the costs to implement exceed its population-level benefits. Rather than suggesting that these conditions should not be treated, these results can guide us to explore how to deliver these important interventions in a more cost-effective manner.
Gaps in evidence for adolescent mental health
A key learning from this investment case study was about the limitations of the current evidence base. Almost all the evidence on intervention design and effectiveness comes from high-income countries (HIC). While we were able to adapt estimates around the cost of delivering interventions in each country, we did not make changes to the estimated effect size or program design in different countries. Nonetheless the dearth of low- and middle-income country (LMIC) studies limits the degree to which interventions can be tailored for implementation in low- and middle-income countries. In addition, there may be important differences in the needs and responses of young people within the adolescent population that should be accounted for in the design of programs. Implementation research is needed to identify how to tailor interventions to meet the needs for example of the most vulnerable adolescents, such as those experiencing violence or lacking housing.
We recommend that governments and global health funders increase their investment in adolescent mental health. To support scaling up these investments, further research is needed to better understand:
- the effects of mental health interventions on long-term outcomes
- how to tailor and scale up mental health interventions in LMICs
- how to reach the most vulnerable young people with mental health interventions
Country-level investment cases for adolescent mental health
We are continuing work in this area by developing national-level adolescent mental health investment cases in five countries (Egypt, England, India, Indonesia, and Mexico). These analyses will adapt our global model to produce country-specific results. Further, we know that economic evidence is only one element of what countries need to inform prioritization and implementation of interventions. For this reason, we are also conducting research to understand the readiness and feasibility of implementing different interventions in each nation, which will add further contextual information to help interpret the results of the investment cases.
Funding for this work was provided by AstraZeneca’s Young Health Programme.
Visit RTI’s Center for Noncommunicable Diseases for more information about our work.
Related Insights:
School-Based Interventions for Adolescent Mental Health | RTI
Adolescent Mental Health in Low- and Middle-Income Countries | RTI