This blog was originally published by The Medical Care Blog.
Last month, the Centers for Medicare and Medicaid Services (CMS) Innovation Center
announced its newest alternative payment model for primary care, Making Care Primary (MCP). MCP builds upon lessons learned from previous CMS primary care models: the Comprehensive Primary Care Initiative, the Comprehensive Primary Care Plus (CPC+) initiative, the Maryland Primary Care Program, and Primary Care First (PCF). CMS will test MCP in 8 states for 10.5 years. It will include Federally Qualified Health Centers (FHQCs), an important type of safety net provider.
We examine below one potential challenge to maximizing the participation of FQHCs in MCP. We found that many FQHCs may not have enough attributed Medicare fee-for-service (FFS) patients to meet MCP’s eligibility requirements. However, we also found that CMS selected states with relatively large FQHCs, helping to mitigate this challenge. Going forward, CMS may want to consider allowing multiple FQHC sites under the same parent organization to participate together. This would enable more FQHCs to be eligible for MCP.
Diversifying the patients in primary care models
Through its primary care models, CMS has made investments to improve the quality of primary care throughout the country. For example, CPC+ provided significant additional funding [PDF] to participating practices, important given the U.S.’s chronic underfunding of primary care. CPC+ also required that practices ensure patients have 24/7 access [PDF] to practitioners, which can be especially valuable to workers without sick leave benefits. However, practices in CMS’s previous primary care models tended to serve Medicare FFS patients who were whiter and more affluent [PDF] than the general Medicare population.
MCP’s inclusion of FQHCs helps address this important limitation. FQHCs generally serve a greater proportion of patients who are socioeconomically disadvantaged [PDF]. The majority of FQHC patients have incomes at or below the federal poverty level. Including FQHCs, and by extension, a more diverse set of patients in these primary care models can help ensure that underserved populations are not excluded from CMS’s investments in primary care. This may help avoid exacerbating existing disparities in access to primary care.
Not all FQHCs will be eligible for MCP
MCP’s inclusion of FQHCs would diversify the patient population for CMS’s primary care models. However, one question arises about how many FQHCs will be eligible to participate in MCP. In 2021, almost half of FQHC patients were enrolled in Medicaid. But only about 11% were enrolled in Medicare, which includes both Medicare FFS and Medicare Advantage patients. However, MCP requires that an organization, including FQHCs, furnish health services to at least 125 attributed Medicare FFS patients. For any particular time period, a patient can only be attributed to one primary care provider. And since patients can visit multiple primary care providers, merely visiting an FQHC site would not ensure that the patient is attributed to the FQHC. Without being attributed, the patient would not count toward the FQHC’s payments under MCP’s payment structure.
CMS often requires a minimum number of attributed Medicare FFS patients. A minimum sample size is required to reliably measure care quality, which is used in calculating how much providers are paid. In addition, providers may be hesitant [PDF] to overhaul the way they provide care in response to an alternative payment structure if only a few of their patients fall under that structure. FQHCs may lack this critical mass of attributed Medicare FFS patients.
New analysis on FQHCs and their Medicare population
In a new analysis, we used data from 2018-2019 to calculate the number of Medicare FFS patients that would be attributed to FQHC sites. We used Medicare FFS claims for services provided by FQHCs and other primary care providers. This enabled us to identify which health care providers each Medicare FFS patient visited during 2018-2019. To restrict non-FQHC providers to those with a primary care specialty, we used data from the National Plan and Provider Enumeration System. We identified FQHC sites using their CMS certification numbers and included visits to other primary care providers in our attribution.
To attribute patients to either an FQHC site or a primary care physician, we used the claims-based attribution method from PCF. This method attributes patients first based on their most recent annual wellness visit (AWV). If a patient did not have an AWV, we attributed the patient to the provider who they saw the most for primary care. We only have Part B carrier claims for a 5% random sample of Medicare FFS beneficiaries. As a result, we restricted our attribution to this sample.
We calculated the number of Medicare FFS patients attributed to each FQHC site. In addition, we examined the distribution in the attribution count nationally and by state. We extrapolated the interim attribution count from the 5% sample to all Medicare FFS beneficiaries. Finally, we conducted sensitivity analyses using three alternative attribution methods used in other CMS alternative payment models: one using only one year of claims, another removing the AWV step, and a third requiring the majority, rather than a plurality, of visits.
Almost 60% of FHQC sites in participating MCP states met the 125-patient threshold required for MCP eligibility
We found 1,924,285 Medicare FFS beneficiaries with at least one visit to an FQHC site during 2018 and 2019. Among the 6,573 FQHC sites in our data for the U.S., we found that the median site had 121 patients attributed. This means that more than half of FQHC sites in our data did not meet the 125-patient threshold for MCP eligibility.
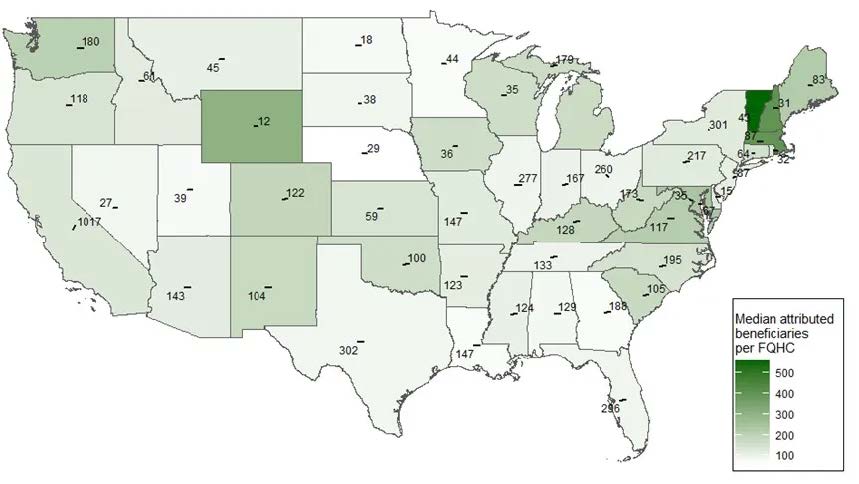
However, we did find large variation across states. Exhibit 1 is a heat map that illustrates the number of FQHC sites in the contiguous U.S. It also includes the median number of attributed Medicare FFS patients per site in each state. We overlay the number of FQHC sites in each state. We also show the median number of attributed patients using the intensity of green for that state. The greener the state, the more attributed patients in the median FQHC site. The median site in the top three states of Vermont, New Hampshire, and Massachusetts had 558, 399, and 397 patients. The median site in 26 states had fewer than 125.
Exhibit 1. The count of FQHC sites and median number of attributed Medicare FFS patients by site, 2018-2019
We also focused on the eight states announced as part of MCP. Exhibit 2 shows the number of FQHC sites with at least 125 Medicare FFS patients for each state. We found that the number of FQHC sites with at least 125 Medicare FFS patients ranged from 16 in Minnesota to 146 in New York for a total of 634 FQHC sites across these 8 states. This represents almost 60% of all FQHC sites in these states. Our results did not change significantly using our alternative attribution methods. However, we did not assess all attribution methods. CMS could use some other attribution method for MCP that may yield higher numbers of attributed patients for FQHCs.
Exhibit 2. The number of FQHC sites with at least 125 Medicare FFS patients in MCP states
| State | Number of FQHC sites with at least 125 Medicare FFS patients | Total number of FQHC sites | Percent of FQHC sites with at least 125 Medicare FFS patients (%) |
|---|---|---|---|
| Colorado | 75 | 122 | 61 |
| Massachusetts | 66 | 87 | 76 |
| Minnesota | 16 | 44 | 36 |
| New Jersey | 39 | 87 | 45 |
| New Mexico | 64 | 104 | 62 |
| New York | 146 | 301 | 49 |
| North Carolina | 105 | 195 | 54 |
| Washington | 123 | 180 | 68 |
| Total | 634 | 1120 | 57 |
Conclusions
CMS’s inclusion of safety net providers like FQHCs in MCP is an important step in extending its efforts to improve primary care and achieve health equity for underserved patient populations. We highlight here one challenge that CMS may face in including FQHCs: the lack of a critical mass of attributed Medicare FFS patients. We found that less than half of all FQHC sites, nationally, have enough attributed Medicare FFS patients to meet CMS’s 125-patient threshold to be eligible to participate in MCP.
However, we also found large variation across states. Given this variation, CMS selected eight states with relatively large FQHCs. In these eight states, almost 60% of FQHC sites meet the 125-patient threshold. In addition, some states selected by CMS, such as Washington and Massachusetts, include FQHCs with experience participating in Medicaid alternative payment models. Separately, recognizing the importance of Medicaid to FQHCs, CMS is working with state Medicaid agencies to bring in Medicaid patients, which comprise almost half of FQHC patients.
Going forward, CMS plans to issue a request for applications to MCP later this summer. It will then launch MCP on July 1, 2024. CMS may want to consider additional measures to maximize FQHC participation in MCP. In particular, CMS could consider allowing multiple FQHC sites under the same parent organization to participate together. This would enable more FQHC sites to meet the 125-patient threshold. Making these important decisions in the design of this new model can potentially lead to lasting impacts for the most underserved patients in the next decade and beyond.