
Insights
Ensuring Quality as Use of Telehealth Expands Due to the Coronavirus Pandemic
Telehealth is the interactive, electronic exchange of information for diagnosis, treatment, support or care management. With telehealth, medical information is generally shared through two-way audio and video and through other telecommunication technology—including mobile communication devices and remote monitoring devices—with the goal of improving a patient’s health status. Telehealth can enhance access to care and improve outcomes by overcoming geographical barriers and workforce challenges.
Telehealth uptake is hindered by issues of licensing and credentialing, types of services and providers eligible for reimbursement by payers, restrictions around prescribing, and technology. Due to the coronavirus pandemic, various federal agencies have temporarily changed policies to expand access to telehealth. The Centers for Medicare and Medicaid Services has expanded reimbursement for telehealth services, and many private payers have followed suit. The Office of Civil Rights has temporarily allowed for consumer-facing technologies such as FaceTime and Skype to conduct telehealth transactions. The Drug Enforcement Administration has issued guidance allowing approved providers to prescribe certain controlled substances without first having an in-person visit. All of these changes were designed to expand access to telehealth and keep patients out of health care facilities due to social distancing. As a result of these changes, payers and providers have expanded their telehealth offerings.
Due to social distancing, many providers have moved the bulk of their care to telehealth visits. As telehealth uptake continues to increase, providers and payers will shift their focus from implementation to the evaluation and use of telehealth. This focus will include understanding the quality of telehealth visits and impacts on existing health care quality measures. After social distancing is over, decisions will need to be made by both payers and providers about parameters for telehealth visits going forward. There are a number of factors for both policymakers and health care executives to consider, including patient satisfaction and demand, cost, quality, and outcomes.
Patients who are homebound, immunocompromised, or in remote areas may wish to continue with telehealth services to improve their access to care. Additionally, patients who want the convenience of telehealth to save time by reducing travel or to quickly access care after-hours may continue to seek virtual care if it’s available. However, telehealth is not necessarily appropriate for every encounter, so providers and payers will need to develop parameters around visits. Items to consider for new parameters include patient diagnosis, the type of visit, the type of provider, and the patient care trajectory.
In order to develop parameters, lessons can be learned from the current high-speed, high-volume implementation of telehealth. Providers are using resources such as the American Medical Association’s Digital Health Implementation Playbook and the Maryland Health Care Commission Telehealth Readiness Assessment toolkit—which RTI helped develop—to support telemedicine implementation.

Providers are using resources such as the American Medical Association’s Digital Health Implementation Playbook and the Maryland Health Care Commission Telehealth Readiness Assessment toolkit—which RTI helped develop—to support telemedicine implementation.
Both resources include some guidance to support evaluation and continuous improvement after they’ve implemented these services. RTI’s telemedicine experts can also assist providers through the identification of telehealth services to maintain after the pandemic, continuous quality improvement of telehealth, evaluations of outcomes of interest, and calculation of return on investment for the successful implementation and use of telehealth services.
Providers need to carefully monitor patient and provider engagement and quality of care delivered through telemedicine to avoid poor health outcomes and potential financial loss in the future. This is especially true for the growing number of health care organizations that are part of value-based payment arrangements who risk financial reimbursement loss if they do not provide good quality of care. While Medicare’s Meaningful Measures Framework of priority areas of quality measure development can be used as a guide, another resource previously created to support measuring telehealth quality is the National Quality Forum’s (NQF) quality framework. NQF suggests assessing telehealth quality through evidence-based measures of four major domains, including:
- A patient’s access to care, the clinician’s access to appropriate technologies and services, and both the patient and provider’s access to relevant clinical information
- Financial impact (e.g., the cost savings or burden) of telemedicine to the patient, care team, payer and/or health system, and to society
- Experience and effectiveness of virtual care for providers, patients, and the community
- System, clinical, operational, and technical effectiveness of telehealth treatment and technologies
RTI’s quality measure experts understand the multiple factors to consider with health care quality and can assist providers in measuring quality of telehealth services in the post-COVID-19 pandemic world. Our experts have led research studies for quality measure calculation and technical specifications for providers in accountable care organizations as well as development, maintenance, and public reporting of quality measures for post-acute care settings for Medicare.
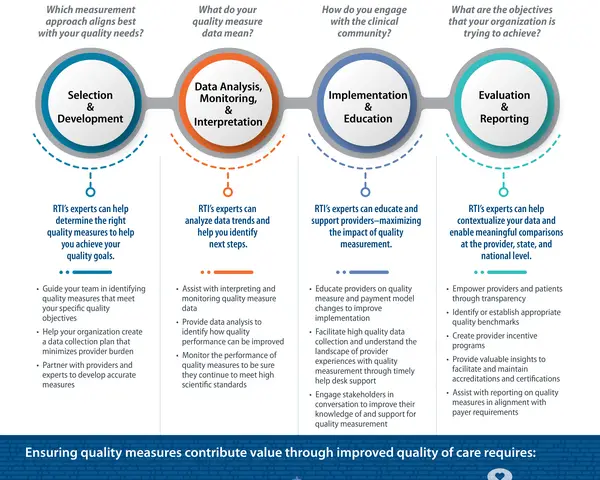
Quality Measurement
To improve quality of care through quality measures, you must choose the right measures, ensure accuracy, and minimize burden. Learn more about how RTI experts can help with any stage of your quality measurement.
Our researchers and clinicians have worked extensively to understand the key challenges of providers across different settings and the amount of time needed for quality measurement implementation; we can apply that knowledge to quality measurement of telehealth.
RTI’s experts also have the capabilities to modify or develop quality measures for telehealth applications whose reliability and validity have been previously tested for in-office visits or institutional settings. For example, new structural quality measures may need to be developed to assess a health care organization’s telehealth capacity, while current process measures may need to expand who is included in a quality measure for virtual assessments, such as patients whose blood sugar is remotely monitored by primary care providers. Certain web-based patient-reported outcome measures (PROMs)—such as the Focus on Therapeutic Outcomes PROMs—may not require substantive alterations to their quality measure specifications, while other PROMs that rely on in-person interaction may.
While we do not yet know how widespread telemedicine will be implemented by providers once the COVID-19 pandemic is over, there are key opportunities that health care organizations can learn from its rollout during social distancing that may inform issues around future adoption. Provider input and careful evaluation of the data collected during this time on telehealth implementation and its effects on patient quality and outcomes will inform changes that are needed to improve both health care quality and quality measures—as well as the future decisions of policymakers and key stakeholders. RTI’s telemedicine experts—with an extensive background in telehealth readiness, evaluation, technical assistance and policy analysis—and quality measurement experts—with a deep history of developing, testing, and maintaining complex quality measures—will continue to monitor changes to the telehealth landscape and impacts on quality measurement as the COVID-19 pandemic evolves.
Learn more about how telehealth is being leveraged during the COVID-19 pandemic.
View Additional RTI Quality Measurement Experts
Disclaimer: This piece was written by Saira Haque (Director, Data Interoperability and Clinical Informatics) and Molly Vaughan to share perspectives on a topic of interest. Expression of opinions within are those of the author or authors.







