Clinical Trial Results that Tested Behavioral and Communication Interventions to Help People Manage Opioid Prescriptions for Chronic Pain
Objective
Conduct a large pragmatic, randomized trial to test two behavioral interventions for people experiencing chronic pain on voluntary opioid reduction.
Approach
Patients at three health systems in North Carolina and Tennessee were assigned to either: (1) motivational interviewing plus group cognitive behavioral therapy sessions (MI+CBT) or (2) individual shared decision-making (SDM) discussions with clinicians as part of their routine medical care. The interventions aimed to educate patients, provide coping skills (CBT), and improve communication around their treatment related values and preferences (SDM). We collected data from electronic health records about prescribed opioid dosage and self-reported pain interference on daily life and physical functioning at 6 and 12 months. Qualitative data via patient interviews and focus groups supplemented the quantitative data.
Impact
Decreases in opioid dosage at 12 months were generally small and did not differ by intervention group. Self-reported physical function and pain interference at 12 months did not change for either group. However, MI+CBT was effective at reducing opioid dosage among patients who had a diagnosed mental condition (anxiety or depression). Patient engagement in this research was essential along with patient feedback about prominent educational materials for chronic pain patients which indicated that they need to be continuously updated and tested to ensure that they are patient centered and not stigmatizing. Future funding for this work is critical. View the published manuscript.
Chronic Pain and Opioid Use
Chronic pain—or pain that lasts for months or years—is one of the most common health problems in the United States. About 20% of American adults suffer from chronic pain (not related to cancer).
Clinicians commonly treat chronic pain with opioid medications. While these treatments can help ease pain in the short term, evidence for their effectiveness in the long term is weak. Further, for some people, opioids can lead to addiction and overdose.
People in pain need effective options to help manage symptoms so that they can enjoy life as much as possible. Behavioral interventions, such as cognitive behavioral therapy, can help patients achieve this goal.
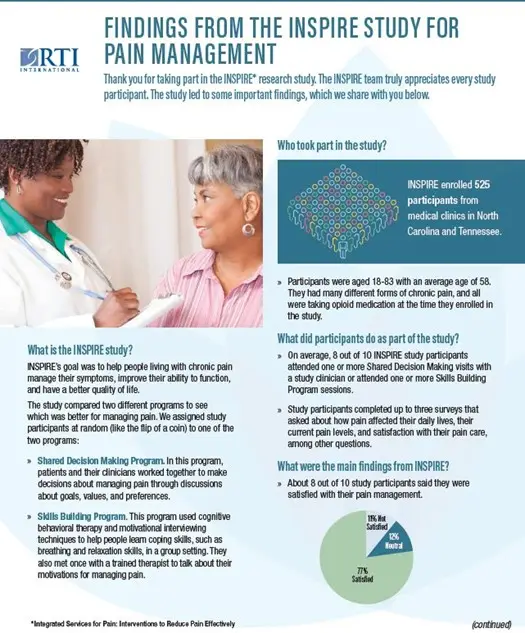
The INSPIRE Trial
INtegrated Services for Pain: Interventions to Reduce Pain Effectively (INSPIRE) compared two programs for helping people living with long-term pain. To take part in the study, people needed to be taking opioid medication for three or more months. INSPIRE enrolled 525 participants across medical clinics in North Carolina and Tennessee. Study sites and Co-Investigators were affiliated with Duke University, University of North Carolina at Chapel Hill, and Vanderbilt University Medical Centers. INSPIRE also relied on patient partners—people who had lived with pain—to provide valuable input throughout the study.
Interventions and Outcomes

Study staff and clinicians developed an 8-session, group-based cognitive behavioral therapy (CBT) intervention for pain, based on standard CBT curriculums. CBT is a structured and goal-oriented approach that helps people change negative feelings, thoughts, and behaviors. CBT participants learned about topics such as breathing, relaxation, pacing, planning pleasant activities and applied these techniques through activities. Most sessions were held virtually and led by trained therapists. Prior to starting CBT, participants had an individual motivational interview (MI) session with a therapist to talk about their pain management goals.
The shared decision-making (SDM) intervention involved a two-way exchange of information, goals, and preferences between study participants and their clinicians. SDM discussions occurred during regular clinic visits with a goal of enhancing communication. INSPIRE clinicians received SDM training and patients received educational information in the form of worksheets, handouts, and a video about pain management and opioids.
We collected information from patients’ health records on their opioid prescriptions over the study duration. In addition, study participants completed online surveys at enrollment, 6-months, and 12-months about pain outcomes, such as how pain interfered with daily living and their overall physical functioning. Qualitative data via patient interviews and focus groups supplemented the quantitative data.
Insights about Pain Management Interventions
Key insights include:
- Overall, decreases in opioid dosage were small after participating in the interventions.
- However, among study participants who had a diagnosed mental disorder—such as anxiety or depression—the MI+CBT intervention showed greater reductions in opioid dosage compared to the SDM intervention. This subgroup did not report worse pain outcomes alongside their dose reduction.
- Although helpful for initiating conversation with their doctors, participants felt that the SDM educational materials could be updated to touch on novel pain treatments and the social and emotional aspects of pain. Some participants thought the educational materials could be improved to avoid potential stigmatizing language when describing opioid-related harms.
“I felt like I was in a group of people who understood what I was going through. Nobody had this same condition, I don't think any two people even had the same thing. But everybody understood what it's like to live in pain, the isolation, the depression, how it affects your life. That was one of my favorite things...that I didn't feel as alone.” - Study Participant, CBT group
What this Means for Clinical Practice
Effectively managing pain remains a challenge, and any single behavioral intervention may yield only small effects on outcomes like opioid reduction and pain interference. Patients need multiple available strategies to support them. Behavioral interventions—like group CBT—can help some patients support their goals.
What this Means for Pain Education
Patient education materials can be helpful resources, but they need to be current, appropriately timed, and patient-centered.
This work was supported through a Patient-Centered Outcomes Research Institute (PCORI) Project Program Award (OPD-1610-37006). Comparing Two Ways to Help Patients Manage Long-Term Non-Cancer Pain | PCORI PI: Lauren McCormack
Collaborators:
- Duke University School of Medicine
- University of North Carolina at Chapel Hill
- Vanderbilt University Medical Center
- Project Lazarus
Clinical Trial Identifier: NCT03454555




