FDA Approves Pretomanid for Treatment of XDR-TB
During the 20 years that she has been leading RTI’s work to find better treatments for tuberculosis (TB), Doris Rouse sometimes found herself pounding on her desk exclaiming to staff, “Someone is dying every 15 seconds from this disease,” to emphasize the critical importance of the work.
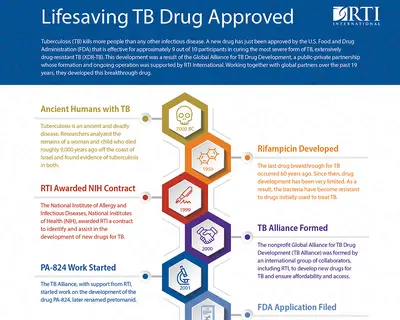
But as the project manager for the public-private partnership that identified pretomanid, only the third anti-TB drug approved by the U.S. Food and Drug Administration (FDA) in more than 40 years, her dedication and passion have paid off. The FDA announced approval of the drug this week.
Pretomanid, a treatment for extensively drug-resistant TB (XDR-TB), was developed by TB Alliance, a non-profit public-private partnership that RTI helped to form in 2000. XDR-TB is a type of TB that is resistant to two of the four main drugs that are given for TB around the world, plus any fluoroquinolone and one or more of three injectable second-line drugs.
“Although an ancient disease, tuberculosis is a major threat in the 21st century,” Rouse said. Currently, tuberculosis kills 1.6 million people a year—more than 4,000 people a day. In fact, it is killing more people than any other infectious disease. XDR-TB is a major and growing threat to the world.” The World Health Organization (WHO) has reported that 129 countries (including the U.S.) have reported at least one case of XDR TB.
The drug shows success for approximately 9 out of 10 participants in curing XDR-TB, with a 6-month treatment period when combined with two other oral drugs. Current treatment takes 18 months or more with less than half this level of success.
To fulfill its mission to provide affordable and accessible treatments, TB Alliance has negotiated license agreements enabling a lower cost for pretomanid in low-resource countries.
A Long Path to More TB Treatment Options
With funding from the National Institute of Allergy and Infectious Disease (NIAID), in 1999 Rouse and a team at RTI headed up the effort to identify potential new compounds for TB treatment. They identified and conducted due diligence on pretomanid, a compound developed by a small biotech firm. RTI assisted TB Alliance in planning and managing the preclinical studies needed for development and preparing the successful Investigational New Drug (IND) application to FDA in 2005, leading to the start of clinical trials that year. RTI has served as a regulatory contact for TB Alliance since that time.
“We’ve worked on this for 19 years, and it hasn’t always been an easy path,” Rouse added. “But as I’ve always said, ‘One of the main ingredients for successful drug development is blessed stubbornness.’ Along this journey, we felt that this was a promising enough drug that we had to try whatever we could to make it a success. There were too few good options.”
Rouse first encountered global health challenges when she began work in Liberia with the Peace Corps in 1970.
“I had no awareness of TB before then,” she noted. “My best student in Liberia contracted cerebral malaria, and he was never the same. I visited a leprosy treatment center there, and that was very difficult. It was that exposure that made me realize the disparity of health care in low-resource areas compared to wealthy nations. There was nothing like being there on the ground and seeing it.”
A History of Public-Private Partnerships
Before Rouse, who is a chemist by training, began working with TB Alliance, she had been working to develop public-private partnerships to take NASA technology and apply it to medical devices.
She was approached after giving a presentation about these types of partnerships from someone who wanted to bring together different sectors to tackle the treatment of TB.
She wrote a proposal, and in 1999 RTI was awarded a $5 million, seven-year contract by NIAID to identify and accelerate the development of new TB treatments.
RTI assisted in the planning and presentations at a February 2000 meeting in Cape Town, South Africa, that led to the formation of TB Alliance. With the funding from NIAID, Rouse and her RTI team supported TB Alliance by conducting due diligence on the early results for pretomanid, preparing the preclinical development plan for pretomanid and serving as the preclinical program manager.
“This public-private partnership is an excellent model for meeting unmet needs, especially those that are in low-resource countries that may not have the commercial attraction that other diseases might have,” Rouse added. “That was the case with tuberculosis. The international community realized developing a new drug required combining resources and expertise from industry, government and the nonprofit sector.”
Tackling TB Drug Resistance
Rouse and team were tasked with identifying promising new compounds. They identified a new class of compounds in 2000 that they thought could be used to treat TB and TB that was resistant to traditional TB drugs. Resistance was growing largely because of inappropriate treatment or noncompliance by patients to the strict daily regimen, which required taking four drugs over a six-month period. Patients begin to feel better before the prescribed end of treatment and sometimes stop taking the drugs, or drugs are not available, leading to multi-drug and XDR-TB. Like other forms of TB, XDR-TB can be transmitted by airborne droplets from a person infected with TB.
In addition, because many of the countries with large populations of TB may not have the infrastructure to diagnose XDR-TB, the exact number of cases is not known. WHO estimates there are 39,000 cases worldwide of XDR-TB, but only 8,700 of those are being treated, so the incidence could be much higher. And because one in every three people worldwide is estimated to have been exposed to TB, the need for new treatments could grow in the future, Rouse noted.
During development, the team encountered some challenges, such as the limited solubility of the compound, which is critical to offering it as a pill. In addition, the initial synthesis of the drug was complex and expensive.
But they conquered those obstacles, and now, instead of pounding on her desk, Rouse—whose colleagues have called her TB work her “third child”—gets emotional when she recounts the 20-year journey to pretomanid.
“Having pretomanid approved and now available for extensively drug-resistant treatment is really the most impactful thing I could have ever imagined doing in my career,” Rouse noted. “And I feel very fortunate and privileged to have had the opportunity to do this work with the wonderful staff here at RTI, with TB Alliance and the patients worldwide, all of whom contributed to the advancement of this important drug. And now it’s available to treat people who really have no other good option for a cure.”
- Global Alliance for TB Drug Development