Modeling health benefits and financial costs of diabetes interventions
For those with chronic diseases like diabetes, it is essential to control blood glucose and address other risk factors to mitigate the long-term complications resulting from the disease. However, though the financial costs of controlling risk factors may be immediate, the health benefits of control accrue gradually over time. Therefore, it is important to understand whether the long-term health benefits associated with an intervention outweigh the costs.
To better understand long-term health benefits and financial costs, RTI, together with the Centers for Disease Control and Prevention (CDC), developed, integrated, and deployed new chronic disease simulation models that more effectively predict risk factors and complications for type 1 diabetes, type 2 diabetes, and prediabetes. Using Python, the new comprehensive type 2 diabetes and prediabetes models improve on previously developed models by using newer data from U.S. studies, including the National Health and Nutrition Examination Survey, to reduce the incidence and prevalence of diabetes complications. This enables scientists and researchers to work at a granular level and with greater accuracy in the fight against diabetes.
Through these simulation models, researchers can:
- Predict the incidence of complications
- Devise interventions to prevent complications quickly and effectively
- Account for the role of risk factors like age, weight, diet, family history, blood pressure level, cholesterol level, and smoking status in the disease’s progression
- Predict benefits and costs of interventions
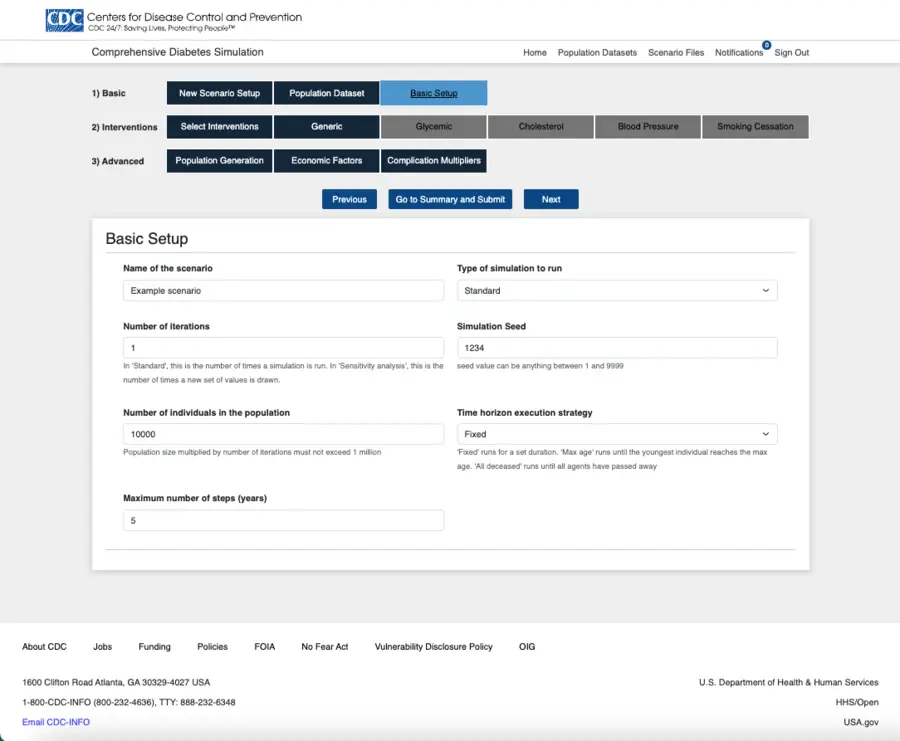
The user interface for running simulation models balances ease of use with flexibility for new and advanced users.
Developing more comprehensive chronic disease models
When the team started the project, CDC’s Division of Diabetes Translation used an existing but limited simulation model to provide insights into type 2 diabetes, which affects 90% to 95% of people with diabetes, and prediabetes, the precursor to type 2 diabetes. However, the model did not account for the 5% to 10% of diabetics with type 1 diabetes.
Simply put, CDC needed more comprehensive models that accounted for heterogeneity—or differences in characteristics—between people with diabetes. Heterogeneity can be achieved with an individual-based simulation model, such as microsimulation.
Drawing from nationally representative de-identified clinical studies, the new type 1, type 2, and prediabetes models apply transition probabilities to simulate diabetes progression among individuals with similar risk factors. The ability to operate at the unit level (in this case, individuals) was a major step forward for CDC and its ability to:
- More confidently understand how risk factors affect specific segments of the population
- Use cost-effectiveness analysis to make more informed decisions about interventions.
Equipped with insights from executing runs of the microsimulation, CDC can use the same input population to compare different sets of health complications and their associated intervention costs to conduct cost-effectiveness analysis.
Applying a secure, user-centric approach to chronic disease models
Building the diabetes risk equations and corresponding simulation models was one aspect of this undertaking. Deploying them was another.
Written in Python, the code to implement these models had to be deployed in CDC’s cloud. This is now a standard requirement across many government projects. Working with CDC’s data science and information technology (IT) teams, the team developed a pipeline that enabled the addition of a suite of automated scans to ensure that the code was secure.
The team was also tasked with developing the system’s user interface to satisfy users at the CDC and outside the organization. Taking a user-centric design approach was essential to ensure the chronic disease models’ usability, and several conversations with CDC proved pivotal in identifying three requirements:
- The system had to be useful. This was the guiding principle for organizing and presenting content, particularly when it came to walking users through the application’s setup process. Embracing an iterative development process enabled the team to refine—and ultimately build in—functionality for sharing and downloading simulation outputs.
- Settings for basic and advanced users were needed. Because the range of users differed considerably, a one-size-fits-all application was not an option. It was critical to give users control of what functionality they wanted to use, striking a balance between flexibility and usability.
- 508 compliance was essential. U.S. law requires federal agencies to make their electronic content accessible to people with disabilities. We are using a tool built in-house, Harness, that has 508 compliance built in and guarantees the models’ continued functionality.
Creating a universal tool for health research and policymaking
The code for these diabetes simulation models has become a valuable tool for researchers because it can be used universally across diseases. As long as there are individuals with attributes that need to be updated at regular intervals, the models can be used for everything from alcohol use disorder to other chronic diseases, such as cardiovascular disease, Alzheimer’s, cancer, and HIV.
The research team is currently working to expand the chronic disease models so they can provide insights into the impact of different health interventions in addressing risk factors and ultimately reduce cases of type 2 diabetes and its complications. The ultimate goal is to use the models to inform health policies to improve health outcomes.
- Centers for Disease Control and Prevention (CDC)