Insights
Model Suggests Newly Admitted Residents Are Unlikely to be the Driver of Nursing Home COVID-19 Outbreaks
Nursing Homes are A Common Location for COVID-19 Outbreaks
With a primarily elderly population, close quarters, and a steady rotation of staff members and visitors, nursing homes are extremely vulnerable to infectious disease outbreaks. Their capacity to manage outbreaks was put to the test during the COVID-19 pandemic. Using data from a period of high case counts during the pandemic, our research team looked to estimate the source of COVID in nursing homes in North Carolina.
Tracking the Source of COVID in Nursing Homes
As of 04/07/2022, more than 21% (4,928 / 23,257) of all deaths related to COVID-19 in North Carolina were from people living in nursing homes. The same data shows that since the pandemic began, nearly 350 COVID-19 nursing home outbreaks have been reported in North Carolina. Tracking the source of outbreaks is difficult, but most experts agree that the presence of asymptomatic carriers and a lack of testing increase the likelihood of a nursing home outbreak. Both staff size and staff networks have also been linked to COVID-19 outbreaks in nursing homes.
Agent-based Models: Simulation Tools to Guide Pandemic Response
During the pandemic, researchers have created numerous data models to forecast COVID-19 cases, hospitalizations, and deaths. Ensemble forecasts, like those hosted through the Centers for Disease Control and Prevention (CDC) COVID-19 Forecasting and Mathematical Modeling hub, leverage model output from dozens of teams across the globe. Forecast accuracy improved as the data used to inform them became more widely available. Decision makers now routinely rely on COVID-19 forecasts to inform public health action. As the pandemic evolves, researchers continue to leverage simulation tools, like agent-based models, to support evidence-based decision making.
What are Agent-Based Models?
Agent-based models are used to simulate the actions of and interactions among computer agents that can represent people.
We created a detailed agent-based model of person movement among North Carolina’s healthcare facilities (e.g., hospitals and nursing home facilities), informed by COVID-19 case and vaccination data. Our model simulates COVID-19 cases, healthcare stays, potential interactions among persons, nursing home visits from family and friends, and healthcare workers at nursing homes. In this agent-based model, COVID-19 cases have one of four severity states:
- Asymptomatic: No symptoms are present; agent behavior is not altered
- Mild/Moderate: Mild symptoms are present; agents less likely to visit friends or family at a nursing home; healthcare workers are less likely to go into work
- Severe: Symptoms require hospitalization in a non-intensive care unit (non-ICU) bed
- Critical: Symptoms require hospitalization in an ICU bed
Each agent in the model has their own COVID-19 state (including not having COVID-19), and this state is updated each day of the model run. Agents within the model have a probability of developing or recovering from COVID-19, as well as seeking care in a healthcare facility throughout the 30-day simulation run.
Assessing the Source of COVID-19 Outbreaks in Nursing Homes
To estimate the likelihood that a newly admitted nursing home resident was the source of an outbreak, we simulated the COVID-19 state of all agents that interact with nursing homes. Our model simulated 427 nursing home facilities located throughout North Carolina and used publicly available nursing home staff data to parameterize healthcare workers providing care within the facilities. Agents entering the nursing home environment include nursing home admissions, nursing home visitors, and nursing home healthcare workers. Peer-reviewed literature informed the social networks of the nursing home residents to simulate nursing home visitation, and data from the Centers for Medicare & Medicaid Services informed healthcare worker staff hours. We do not model COVID-19 transmission within facilities. We ran the 30-day simulation parameterized to the surge in COVID-19 cases related to the Omicron variant (B.1.1.529). Additional modeling details and parameters can be found in our model description document.
Using Simulation Results to Predict the Source of COVID in Nursing Homes
For this simulation, we averaged the results of 10 simulations using model parameters reflecting historical trends during the surge in cases related to the Omicron variant (December 15, 2021-January 13, 2022). Over the 30-day model run, there were ~10,100 nursing home admissions, ~432,000 visitors from the community, and ~522,000 healthcare worker shifts worked. In total, there were ~7,400 agents with asymptomatic COVID-19 and ~4,100 individuals with mild COVID-19 entering the nursing home environment. Only a fraction of all agents with asymptomatic or mild COVID-19 (0.3% and 1.3%, respectively) that entered a nursing home during the model run were nursing home admissions.
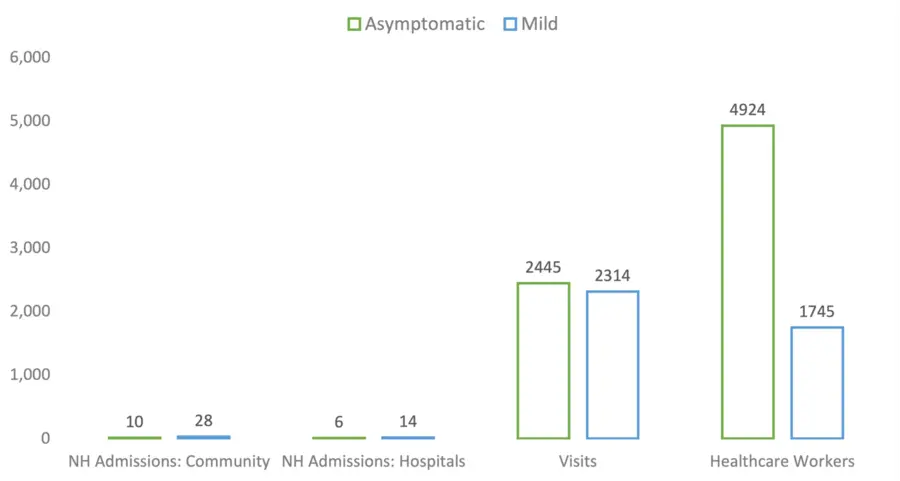
Figure 1. Average Number of Nursing Home Admissions by Type and COVID-19 Status
How Our Modeling Results Can Inform Handling COVID in Nursing Homes
These data modeling results support the idea that the source of most COVID-19 outbreaks within nursing homes are likely asymptomatic or mildly infected healthcare workers or visitors. Nursing home facilities should consider prioritizing prevention efforts that decrease the risk of staff and visitors introducing SARS-CoV-2 into the nursing home environment. The pandemic has caused fluctuations in nursing home admissions from the community as well as from hospitals. Even if 100% of new admissions come from the community (and therefore, have a higher likelihood of SARS-CoV-2 infection) the number of admissions with mild or asymptomatic COVID-19 is only a fraction of the total COVID-19 positive visitors and healthcare workers entering these facilities.
Rate of COVID-19+ Admissions from the Community and from Hospitals
| Nursing Home Admissions From: | 30-Day Run Average | One-Year Estimate | COVID-19+ (Mild or Asymptomatic) Per 1,000 Admissions |
| Community | 1,798 | 21,876 | 20.86 |
| Hospitals | 8,332 | 101,371 | 4.56 |
Disclaimer: This piece was written by Joëlla W. Adams (Epidemiologist), Sandy Preiss (Research Data Scientist), and Sarah Rhea to share perspectives on a topic of interest. Expression of opinions within are those of the author or authors.



