RTI’s National Survey of Syringe Service Programs (SSPs) showed that California’s investment in harm reduction yielded high levels of life-saving interventions in its three years of existence.
The State of California is approaching the end of a three-year program aimed at preventing overdoses and infectious diseases related to substance use. In the summer of 2023, state legislators will consider whether to extend this effort, known as the California Harm Reduction Initiative (CHRI).
About the California Harm Reduction Initiative
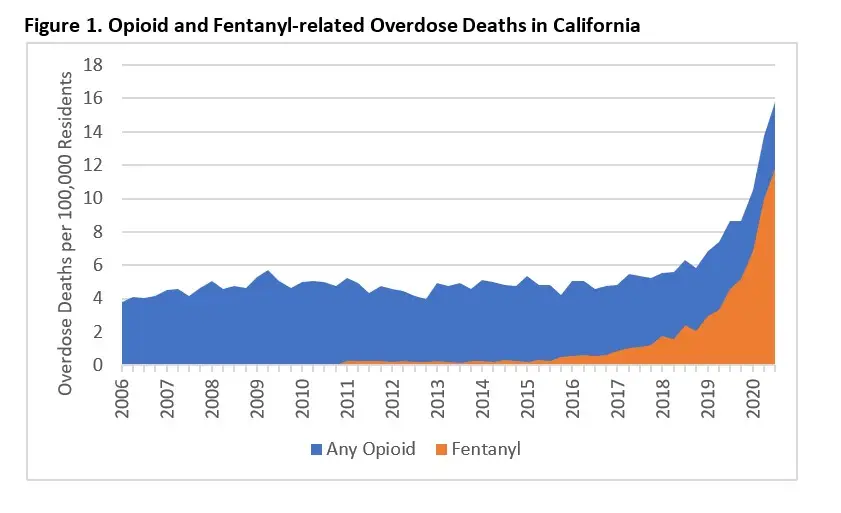
CHRI was a response to steep increases in opioid overdose mortality (Figure 1), and infectious diseases statewide—consequences of the growing presence of fentanyl in the U.S. drug supply. Beginning in August 2020, CHRI dedicated $15.2 million over three years to supporting syringe services programs (SSPs) through direct funding and technical assistance from the National Harm Reduction Coalition (NHRC).
CHRI’s Impact on Syringe Services Programs
Our research found that CHRI was game-changing for SSPs in California, greatly improving their ability to deliver life-saving interventions to people who use drugs. Our team at RTI consists of experts in public health and harm reduction with experience in California and across the U.S. We have been studying the impact of SSPs with funding from Arnold Ventures and in collaboration with researchers at the University of Miami, University of Southern California, and the North American Syringe Exchange Network. Our findings are relevant to the ongoing discussion in California, and to the experience of other states considering ways to mitigate the health consequences of opioid use.
CHRI Funding Helped SSPs Reach and Protect More Californians than Ever
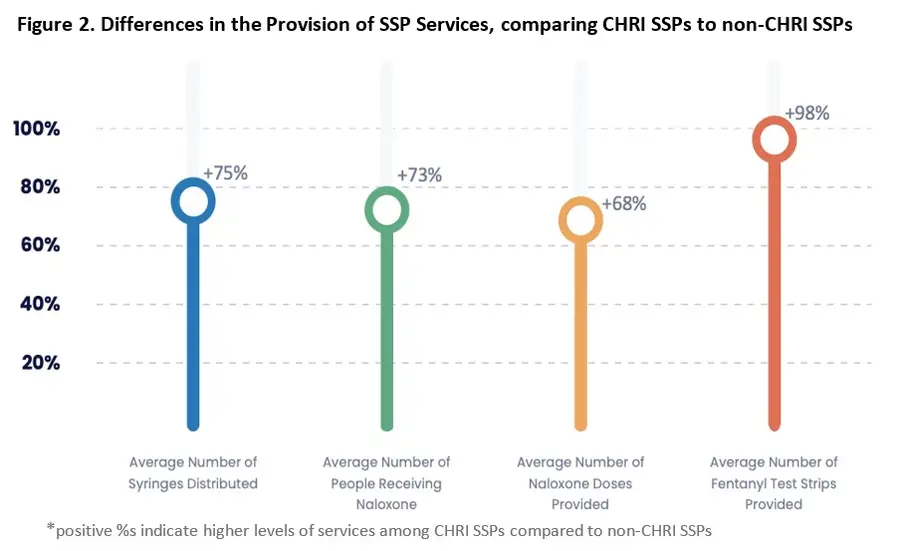
Figures 2 and 3 show the impact that CHRI had on improving SSP-related services in California. On average, CHRI-supported SSPs served 7,905 participants in 2021, compared to 3,360 for non-CHRI SSPs, and provided 75% more syringes than other SSPs in the US. Programs supported by CHRI also provided more naloxone to their participants than other programs. Naloxone can easily be used by someone to quickly reverse an opioid overdose that might otherwise be fatal. CHRI-supported SSPs gave naloxone to 73% more people and distributed 68% more naloxone doses than other SSPs. On average, SSPs supported by CHRI also gave out nearly double the number of fentanyl test strips, which are small point-of-care test strips that can people who use drugs detect whether fentanyl is present in drug solutions.
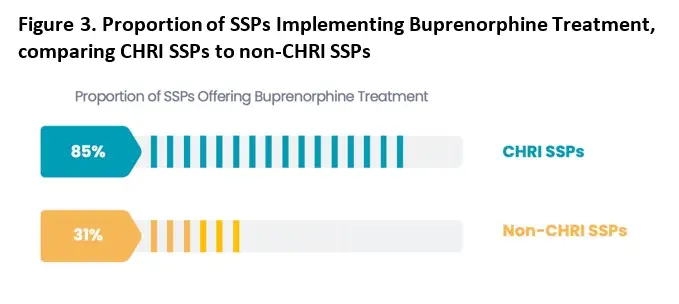
Furthermore, SSPs are ideal settings to integrate buprenorphine treatment for people who have an opioid use disorder (OUD) and are interested in treatment. Buprenorphine is a medication that allows people with an OUD to reduce their opioid use without having to visit a specialty clinic on a daily basis, and reduces the risk of opioid-involved overdose deaths. In 2021, 85% of CHRI-supported SSPs offered buprenorphine to their participants, either through in-person consultations or telemedicine, compared to only 31% of non-CHRI SSPs.
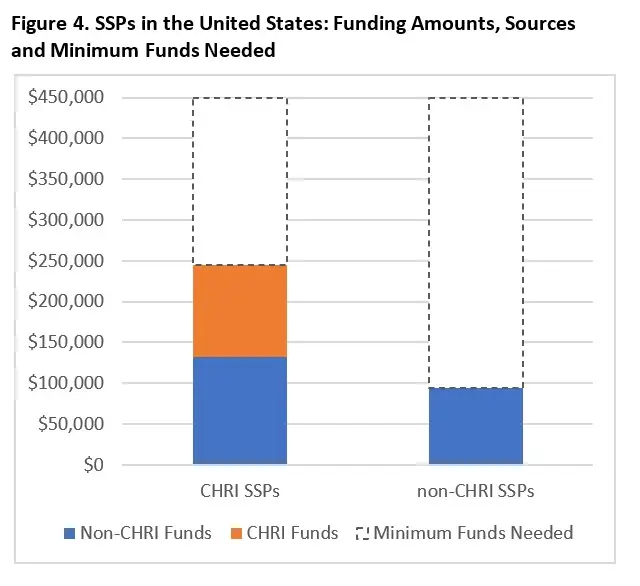
With regards to budget impacts, CHRI-funded SSPs had a median annual budget of $245,000, approximately $150,000 more than the median annual budget among other SSPs in the United States ($93,920). The median budget per SSP provided by CHRI was $112,500, which accounted for the majority of budget differences compared to other SSPs in the United States. Yet, with these levels of funding, CHRI-funded SSPs are still funded 46% below the minimum levels of costs that scientists at the CDC recommend for small, rural SSPs ($450,000). (Figure 4)
Taken together, these findings demonstrate the substantial impact that the funding and technical assistance provided through CHRI has made on SSPs in California. In the context of a major overdose mortality crisis, these results show that the initiative helped SSPs distribute more syringes, naloxone, and fentanyl test strips, and drastically improved access to substance disorder treatment.
What are SSPs, and how do they operate in California?
Per the Centers for Disease Control and Prevention, SSPs “are community-based prevention programs that can provide a range of services, including linkage to substance use disorder treatment; access to and disposal of sterile syringes and injection equipment; and vaccination, testing, and linkage to care and treatment for infectious diseases.” The 37 SSPs funded by CHRI were located throughout the state and received up to $150,000 per year for 3 years (Figure 2), making CHRI the largest single investment in harm reduction ever made by the State of California.
In addition to direct funding, each CHRI-funded SSP was assigned a technical assistance provider at NHRC, who offered regularly accessible office hours and structured quarterly calls for grantees to voluntarily attend. In coordination with the California Department of Public Health Office of AIDS, NHRC also offered 21 training sessions for CHRI-funded SSPs, on topics such as hiring and staff support, expanding services, and organizational development. SSPs could also join monthly or bi-weekly mentorship groups, designed to sustain collaborative learning, skill sharing, and emotional support among peers. Technical assistance was also provided through an online listserv among all programs and an annual in-person conference.
Our Approach –National Survey of Syringe Service Programs (NSSSP)
As part of our research on the impact of state-level policy initiatives on service delivery from SSPs, RTI has carried out the National Survey of Syringe Service Programs annually since 2021. In this survey, we contact all known SSPs operating in the U.S. over a six-month period. To reach these SSPs, RTI works closely with the North American Syringe Exchange Network (NASEN) to recruit programs from their database, which they have continuously maintained for the last 30 years.
Organizational directors from SSPs were initially emailed up to three times asking them to participate in the survey, and for those who did not respond, additional follow-up with individual programs was conducted via phone calls. SSPs were offered a $75 honorarium for completing the survey. For this analysis, we included data from our survey conducted February to July 2022, which included information about SSP operations in calendar year 2021. In 2022, RTI achieved a 72% response rate for the NSSSP. The survey included questions about their SSPs’ budget, funding sources, staffing levels, areas of operation, syringe distribution, naloxone distribution, fentanyl test strip distribution and buprenorphine treatment implementation. We combined these data with publicly available data with regards to which SSPs received CHRI funding. Our analysis compared CHRI-funded SSPs to other SSPs throughout the country.

