
St. Helena, one of the world’s most remote inhabited islands, is best known as the place where Napoleon was exiled. Perhaps less widely known is the fact that noncommunicable diseases (NCDs) account for a large share of ill-health and mortality on this tiny island in the South Atlantic Ocean, with data from 2017 suggesting that one fifth of the population were diabetic, and potentially half of adults were hypertensive. Obesity and tobacco use were prevalent, with findings suggesting that almost 7 in 10 patients were overweight or obese and 48% of young adults in their twenties smoked. In addition, island policymakers began to perceive the compelling economic and sustainable development case for reducing NCDs. The island receives overseas development funding and it was evident that NCDs were straining the island’s capacity to address its health and wider needs.
Despite a small and developing public health infrastructure compared to many countries, St. Helena has made considerable progress against NCDs over the past three years, and recently received an award from the United Nations Inter-Agency Taskforce on Noncommunicable Diseases (UNIATF) for its success in implementing a government-wide strategic approach to reduce NCDs and their risk factors. This is an outstanding achievement for St. Helena, which is competing in a category dominated by much larger national governments.
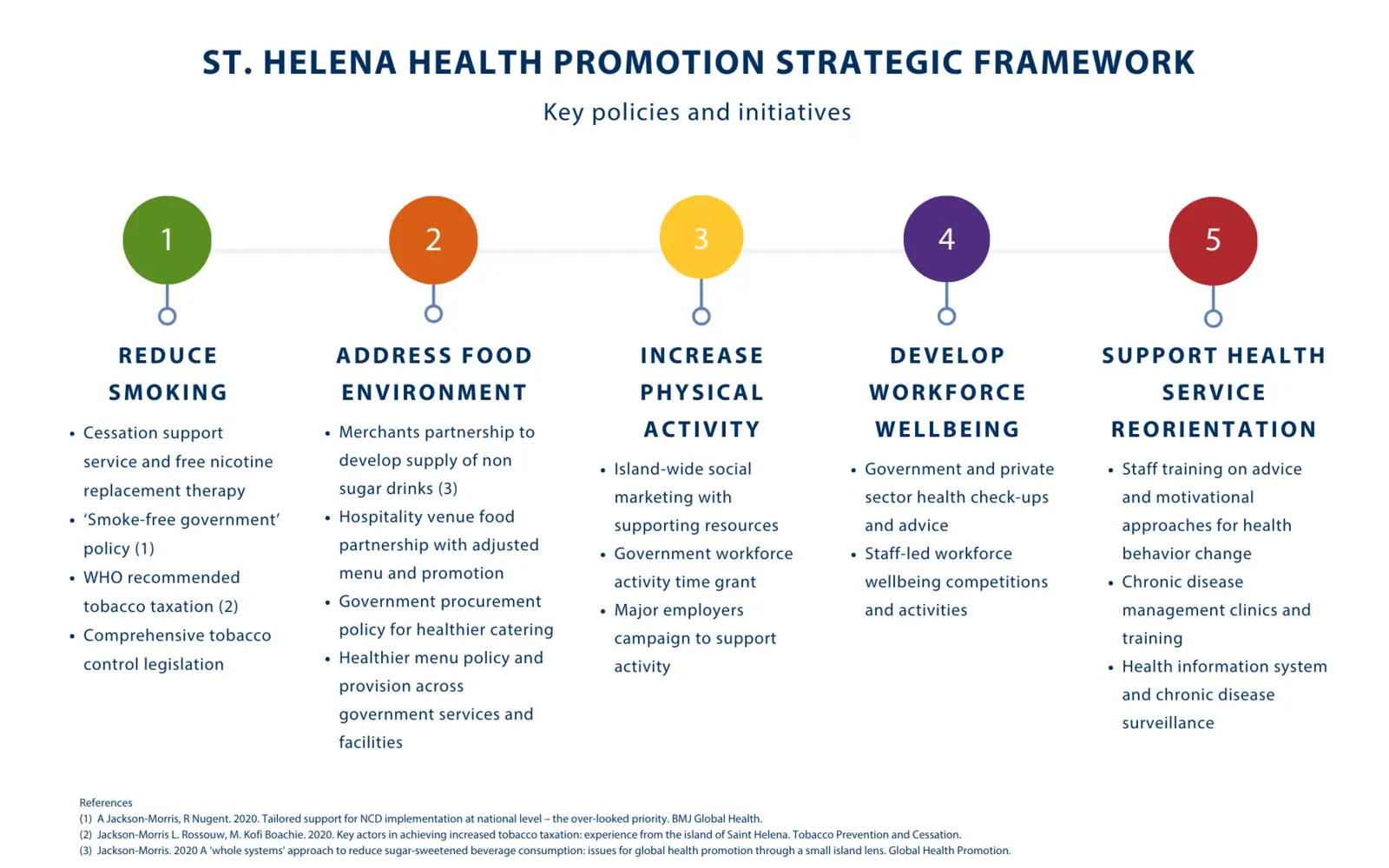
Strategic Framework Helps St. Helena Reduce NCDs
Prior to joining RTI, I was drawn to this small island nation to answer the government’s request for help to address the high prevalence of NCDs by designing tailored solutions based on international evidence. I was attracted by the challenge of addressing the extremely high NCD prevalence and limited public health infrastructure, combined with my belief that the issues were solvable. The starting point in developing the first Health Promotion Strategic Framework 2018-2019 was to understand the issues and context by assessing available national data and identifying gaps, conducting formative research and engaging with a wide range of stakeholders, and reviewing the international evidence. This helped us identify key issues, potentially effective strategies, and perhaps most importantly, how to tailor those strategies to be effective in St. Helena. Delivery was truly collaborative, with all developments undertaken in partnership with different parts of the government, community, and private sector. Health service reorientation developments were led by staff across a range of different disciplines.
By mid 2019, we began to see shifts in health behaviors and risk factors, compared to the established baseline from an island-wide risk factor survey. Data showed a 9% reduction in smoking prevalence and 14% increase in quit intentions, a 26% increase in walking more than an hour weekly, a 13% decrease in sugar-sweetened drink consumption, a 26% decrease in fruit juice consumption – aided by increased government taxation – and a 13% increase in water consumption. The number of people who perceived they ate healthily the ‘majority of the time’ increased by 9%. People increasingly reported their health as ‘good’ as opposed to ‘fair’ and self-perceived control over health increased.
Here are some of the key ingredients that I believe are important to consider when designing and implementing effective NCD policies and programs in low- and middle-income countries, based on my experience in St. Helena and beyond:
- Technical support to assist countries to develop and tailor nationally appropriate strategies that address NCDs
- Building the capacity of national stakeholders such as policymakers, health personnel, and civil society to maximize collaboration with technical support, ownership, and sustainability
- Incorporating ‘whole of government’ and ‘whole community’ approaches to help address different facets of an issue, having a stronger synergistic effect
- Finding solutions that are wins for health but not at the expense of other sectors – for example, using economic modelling to increase taxation while tapering revenue, and working with commercial partners to shift towards healthier provision
- Building multi-sectoral collaboration across the public, community, and private sector to support action across the whole system
- Having an outward-looking as well as context-focused perspective by developing partnerships with specialist external organizations to get advice and support for specific initiatives
- Using community insights and engagement to identify how to make healthier practices easier, move away from unhealthy norms, and encourage buy-in
My hope is that the structural and policy changes that have been put in place in St. Helena will continue to have a positive impact over time, and that the next iteration of health promotion strategies from 2020 onward will help the community make further progress. The early progress we have seen in relation to specific behaviors and environmental changes is tangible, yet they mask perhaps the most important underlying change – that the community itself has begun to take back control of its own health.

