Developing, implementing, and evaluating intervention strategies
According to the 2021 National Survey on Drug Use and Health (NSDUH), more than 61 million Americans reported use of illicit drugs in the past year and 24 million fit the criteria for a drug-related substance use disorder (SUD). People with SUDs face a wide range of negative consequences tied to their drug use, including health issues, disability, social isolation, problems at school or work, and financial strain. However, the implementation of evidence-based intervention strategies is proven to minimize these negative outcomes.
Improving the quality of life and wellbeing of the individual is essential for reducing stigma, limiting fatal overdoses, and keeping drug users as healthy as possible. RTI International understands that trauma-informed, evidence-based interventions are critical for addressing the overdose epidemic. Our experts are on the forefront of research on various intervention strategies—including naloxone distribution, syringe service programs (SSPs), safe consumption sites (SCS), and prescription drug monitoring programs (PDMPs).
Naloxone Distribution
Naloxone has emerged as a critical tool for combatting the epidemic over the last several years, reversing an opioid-related overdose when administered in time. Our researchers are partnering with state and federal agencies to improve the distribution of naloxone, especially for populations at risk for overdose, such as recently incarcerated individuals.
Overdose rates among individuals recently released from jail are more than 100 times higher than among the general population. To combat this growing trend, RTI experts Brad Ray, PhD, and Melissia Larson, MS, led the design and implementation of naloxone vending machines in 32 jails across Indiana, Michigan, and North Carolina. These vending machines increase stigma-free naloxone access for recently incarcerated individuals, visitors, and the general public.
Syringe Service Programs
The overdose crisis is driving a substantial rise in the incidence of infectious disease related to injection drug use, including HIV and acute hepatitis C. SSPs are a key community-based intervention strategy, providing access to clean syringes and syringe disposal for people who inject drugs. These programs are proven to reduce the spread of infectious disease while providing access to substance use treatment, vaccinations, screenings, and other evidence-based interventions.
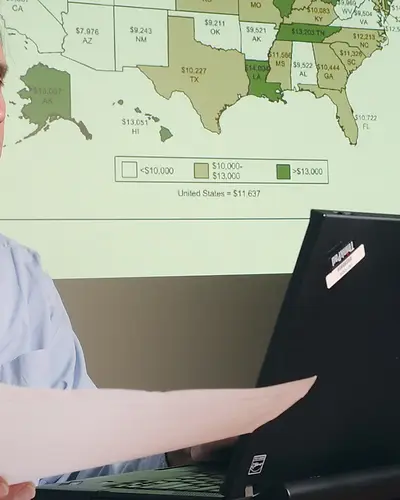
RTI researchers are focused on evaluating the effectiveness of SSPs across the United States to improve future service delivery and save lives. Since 2021, RTI has conducted the annual National Survey of Syringe Service Programs, asking all known SSPs nationwide about their budgets, funding sources, staffing levels, areas of operation, and use of various intervention strategies, including the distribution of clean syringes, naloxone, fentanyl test strips, and buprenorphine.
Safe Consumption Sites
At a SCS, individuals can bring pre-obtained drugs to consume under the supervision of trained staff. Additionally, these sites provide access to clean syringes and have naloxone on hand for overdose situations.
In a prospective cohort study, RTI researchers discovered that access to an unsanctioned SCS resulted in a significant decline in emergency department visits and hospitalization among people who use drugs from 2018 to 2020. The study findings suggest that people with access to SCS may be somewhat less likely to overdose.
Prescription Drug Monitoring Programs
PDMPs are electronic databases that track the prescription of controlled substances. They have emerged as a critical tool for helping health care providers, law enforcement, and other stakeholders address the over-prescribing of opioids. These databases can be used to identify precarious patient behaviors, such as doctor shopping and the illegal sale of prescription drugs, as well as inappropriate prescribing by physicians.
As part of the Prescription Drug Overdose Prevention of States Program, RTI researchers are working with the Centers for Disease Control and Prevention (CDC) to understand how PDMPs are preventing substance misuse and accidental overdose. Through this project, we are collaborating with CDC to combine data from PDMPs across 29 states with NSDUH data, the Treatment Episode Dataset, and the National Prescription Audit to analyze the immediate, short-, and long-term outcomes.