Value-based payment as a strategy for improving care delivery and controlling Medicare Costs
When the Patient Protection and Affordable Care Act (also known as the ACA) was signed into law in 2010, health care’s share of U.S. gross domestic product was at 18 percent and on the rise. Growth in health care spending had exceeded growth of the overall economy since the 1970s. Many people believed that as health care programs required a greater share of the federal budget, it crowded out federal funding for other sectors like education. Yet an expanding body of evidence argued that higher health care spending relative to other developed countries was not translating into proportionate gains in population health. Waste, silos, and inherent incentives of the existing health care financing landscape – depending on provider type and setting – were not only inflating costs of maintaining peoples’ health, but also contributing to poor quality of care for patients due to overprovision or lack of care coordination.
The concept of an accountable care organization (ACO) had been developed and debated among thought leaders in years leading up to the ACA.
The Shared Savings Program’s (SSP) role in transforming health care
While best known for its provisions related to the private insurance market, the ACA also sought to moderate the rate of growth in Medicare spending given Medicare’s large share of the federal budget. Original Medicare’s Parts A and B fee-for-service payment structure lacks financial incentives for providers to reduce unnecessary health care provision or invest resources in better care coordination.
ACOs and Alternative Payment Models
An ACO model is an alternative payment model (APM) that aligns financial incentives of the payer and the providers, leading to a common goal of reducing costs and improving care coordination. Beneficiaries aligned with ACOs can continue to seek care from any provider that accepts Parts A or B Medicare. The Shared Savings Program was established to invite ACOs to form within Original Medicare.
What is a shared savings program?
The Shared Savings Program is a large-scale, national, voluntary program for providers to come together as an ACO and be accountable for the quality and cost of all healthcare furnished to a population of beneficiaries who receive primary care from providers in the ACO.
The ACO is not only accountable for the care furnished by the providers inside the ACO, but also the care furnished to the ACO’s assigned beneficiaries by providers outside the ACO. If the ACO reduces the total cost of care for that beneficiary population through strategies such as improved care coordination, reducing unnecessary care, or introduction of cost savings measures, while also meeting quality standards, the ACO shares the savings with Medicare. The program empowers providers to coordinate efforts through monthly beneficiary data sharing, quarterly reports, and certain billing and referral waivers. The program also aims to encourage improved quality of care through robust quality measurement. A redesign of the quality measurement and scoring methodology will emphasize priority areas of focus around quality of care and minimize reporting burden.
Medicare Shared Savings Program Growth
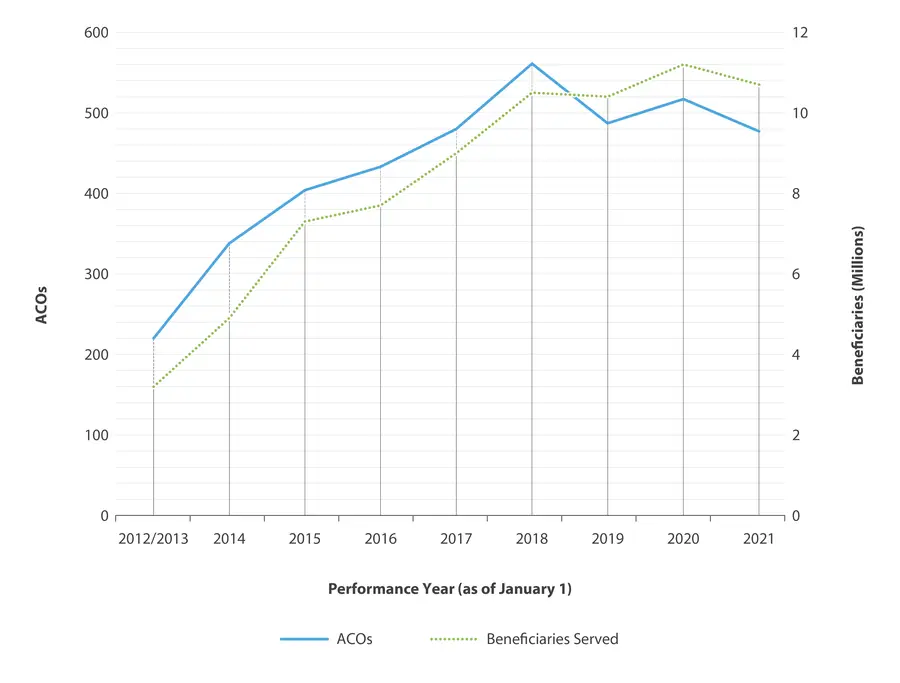
Since the program’s inception, the number of ACOs has grown by 117% and the number of beneficiaries served has grown by 234%.
Delivering on the Promise of Right Care, Right Time, Right Setting
As a research institution with the resources of a large firm, RTI is uniquely positioned to support the client with the most critical and technically complex large-scale operations that are the backbone of the Shared Savings Program. RTI’s elite team employs a wide variety of skills and subject matter expertise: data analytics, economics, and quality of care measurement, to name a few.
RTI supports CMS in administering the Shared Savings Program by:
- Conducting financial calculations that determine ACOs’ shared savings or losses
- Supporting the quality measurement strategy and measuring quality of care
- Managing program data
- Creating the quarterly feedback reports that ACOs rely on to inform their care improvement efforts
- Conducting analyses to inform program administration and design.
In a given year, about one third of all Original Medicare beneficiaries are aligned with an ACO taking accountability for the cost, quality and coordination of their care. ACOs in the Shared Savings Program have achieved lower expenditures for Medicare when compared to benchmarks. The widespread adoption of the shared savings model through this program and others is transforming how providers work to keep the U.S. population healthy.
Medicare Shared Savings Program Financial Performance
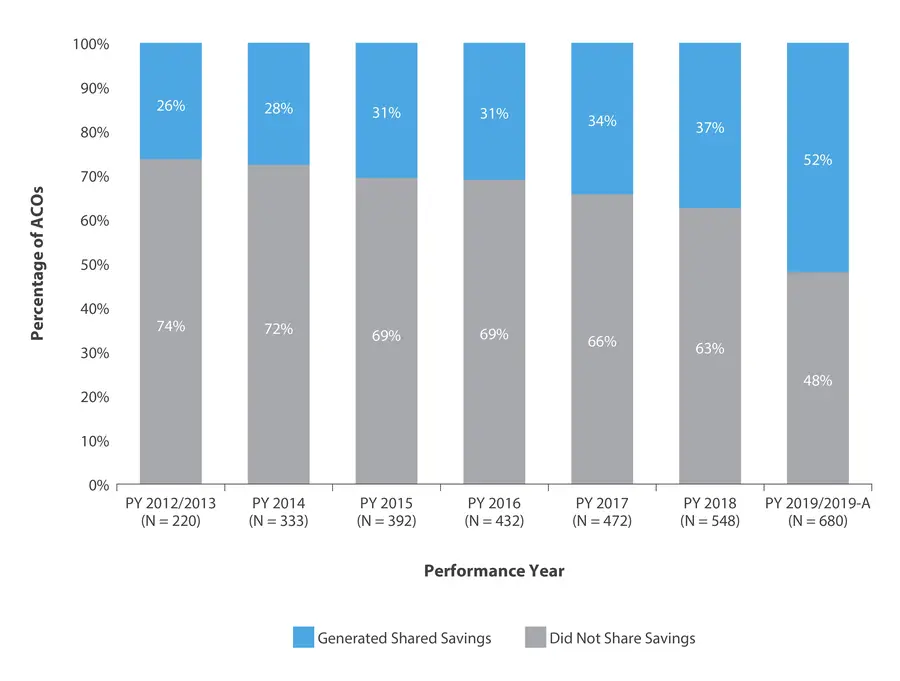
Performance Year (PY) 2019/2019-A saw the highest share of ACOs that generated savings than prior years, showing the success and adoption of this model.
- Centers for Medicare and Medicaid Services (CMS)











