Transforming Primary Care to Improve Health Outcomes and Reduce Health Care Costs
Objective
Comprehensive Primary Care Plus (CPC+) is a value-based care model designed to improve health care for millions of Medicare beneficiaries while reducing health care costs. RTI supported the Centers for Medicare & Medicaid Services (CMS) and approximately 3,000 practices nationwide to implement this model.
Approach
To facilitate CPC+ implementation and operations, RTI developed a detailed technical methodology for all components of the CPC+ payment design. We also supported the CPC+ model in several key areas including technical assistance, practice composition, quality assessment, and policy analysis.
Impact
CPC+ activities enabled primary care practices to transform and improve the care provided to their Medicare and private pay patients. The lessons learned in CPC+ laid the groundwork for the Primary Care First model that followed.
The Medical Home Model: Improving Care and Reducing Costs
Primary care is the foundation of our health care system. It is essential to better health and critical for reducing health care costs. The “medical home” model aims at reorganizing health care so that it is patient-centered and coordinates primary and specialty care, hospitals, home health care, and community services.
Comprehensive Primary Care Plus (CPC+) is a 5-year multi-payer medical home model initiative that began in January 2017 under the authority of the Center for Medicare & Medicaid Innovation (CMMI) within the Centers for Medicare & Medicaid Services (CMS). The model restructures primary care by introducing comprehensive care delivery requirements and an alternative payment design based on patients’ health status and quality of care.
Four Drivers of the CPC+ Model
The CPC+ model is based on four drivers. The program operates in two tracks that differ by care delivery and health IT requirements, as well as by payment structure. The four drivers are:
- Innovative payment design aimed at rewarding provider performance rather than services delivered
- Extensive use of health information technology (health IT), including electronic clinical quality measures
- Care delivery transformation, putting emphasis on five comprehensive care functions: care management, care coordination and comprehensiveness, expanded access, patient and caregiver engagement, and population health
- Continuous improvement driven by patient data on health care utilization, cost, and patient experience
CPC+ Model Scale: Partners, Practices, and Payments
At the time it was implemented, CPC+ was the nation’s largest initiative aimed at transforming primary care. It has involved Medicare and 79 public and private payer partners in 18 regions of the country and engaged 68 health IT vendors. The Medicare arm of the program has been comprised of more than 3,000 primary care practices and 14,000 practitioners, with over 2 million attributed Medicare beneficiaries. In 2020, Medicare CPC+ payments to participating practices amounted to $621,406,954.00.
There are two cohorts of participants: those who started in January 2017 (14 regions, initially 2,905 practices) and those who started in January 2018 (4 regions, initially 165 practices). Model participants include a diverse group of practices that vary in size, ownership, location, and composition of primary care practitioners.
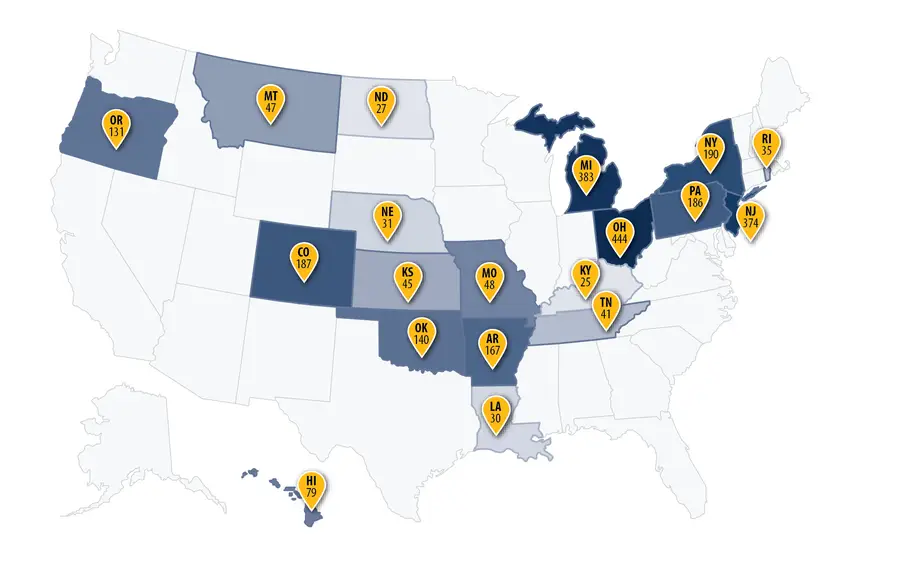
Figure 1. Number of Participating Practices by CPC+ Region. Note: CPC+ has 18 regions across 19 states. The regions are: Arkansas, Colorado, Hawaii, Greater Kansas City Region of Kansas and Missouri, Louisiana, Michigan, Montana, Nebraska, North Dakota, Greater Buffalo Region of New York, North Hudson-Capital Region of New York, New Jersey, Ohio and Northern Kentucky Region, Oklahoma, Oregon, Greater Philadelphia Region of Pennsylvania, Rhode Island, and Tennessee.
Innovative Payment Design Rewards Quality and Offers Flexibility
Medicare CPC+ payment to participating practices has three components:
- a per-beneficiary-per-month care management fee
- a performance-based incentive payment
- a lump sum payment, replacing a progressively larger portion of a practice’s traditional Medicare fee-for-service revenue (for Track 2 practices)
This payment structure rewards accountability and the quality of care provided and offers practices flexibility to deliver services outside of traditional office settings.
Tracking Progress and Calculating Incentive Payments
Several reporting mechanisms are used to track progress toward care transformation and quality improvement by CPC+ participating practices. The practices are required to submit care delivery reporting data and electronic quality measures. These, plus claims-based utilization measures calculated by CMS and the CPC+ Patient Experience of Care survey, are used in calculating the incentive payment as well as in tracking progress.
RTI’s Role in the Development and Administration of CPC+
In addition to developing a detailed technical methodology for all components of the CPC+ payment design, RTI supports CMS’ implementation of the CPC+ model in several key areas:
- Data management – Collecting and storing practices’ data and utilizing the data to provide needed business intelligence to CMS and payer partners
- Monitoring – Overseeing practices’ adherence to the program’s requirements and deadlines, including care delivery, quality, and financial reporting
- Patient attribution – Using an algorithm-based quarterly process of assigning Medicare beneficiaries to practices that are responsible for the majority of their care
- Patient Experience of Care Survey - Collaborating with CMS to design and implement the survey, conduct the sampling, and benchmark results to national data
- Payment calculations – Calculating CPC+ payments based on patient attribution, risk adjustment, and quality and utilization performance measures
- Practice composition – Handling practice management issues, implementing policy decisions related to practice and practitioner participation, and supporting the generation of the practice and practitioner roster—the foundation of practice attribution and payment
- Quality/health IT – Supporting practice use of health IT and certified electronic health record technology, overseeing quality data collection, and compiling results for quality metrics
- Technical support – Assisting participating practices and other stakeholders with communication strategies, including help desk support, a web portal that hosts practice-specific data, and a weekly email newsletter with program announcements and reminders
CPC+ Lessons Learned
CPC+ activities enabled primary care practices to transform and improve the care provided to their Medicare and private pay patients. The lessons learned in CPC+ laid the groundwork for the Primary Care First model, which followed.
- Center for Medicare and Medicaid Innovation