Analyses and development of the prototype Unified Post-Acute Care Prospective Payment System called for in the IMPACT Act
Objective
To build a payment framework across post-acute care (PAC) setting based on beneficiary clinical characteristics rather than type of provider.
Approach
We worked with the Centers for Medicare & Medicaid Services (CMS) and the Assistant Secretary of Planning and Evaluation (ASPE) to construct a prototype for a Unified PAC Prospective Payment System (PPS). We assigned beneficiaries in a uniform manner to one of 4,000+ payment groups based on primary reason for receiving PAC, primary diagnosis, and self-care and mobility functions. The framework includes adjustments for comorbidities, PAC provider type, rural settings, and high-cost outliers.
Impact
Our initiatives align payments and financial incentives with patient needs, which helps move the Medicare program towards a more equitable provision of PAC. This prototype is a significant step towards providing a framework that can be built upon in the future, creating greater Medicare efficiency.
Siloed Payments for Post-Acute Care Create Disparities
Post-acute care (PAC) represents a critical component of the health care delivery system in the United States. Each of the four PAC settings - inpatient rehabilitation facilities (IRF), skilled nursing facilities (SNF), long-term care hospitals (LTCH), and home health agencies (HHA) - plays a distinct and important role in helping Medicare beneficiaries recover after an inpatient hospitalization. Some also care for patients who do not have a prior hospitalization. However, there is considerable variation in the types of patients these settings care for across the U.S., and siloed payment systems can result in Medicare paying very different amounts for otherwise-comparable patients simply because they sought care in different settings.
The Push for a Unified Post-Acute Care Payment System
Researchers at RTI International have been working with the U.S. Department of Health and Human Services Assistant Secretary for Planning and Evaluation (ASPE) and the Centers for Medicare & Medicaid Services (CMS) on activities related to post-acute care payment and quality measurement for over a decade. Most recently, we partnered with CMS and ASPE to develop the prototype for a Unified PAC Prospective Payment System (PPS) required by The IMPACT Act of 2014. The aim was to build a framework that could be used across PAC settings and that would set payment based on beneficiary clinical characteristics rather than type of provider. This work culminated in a Report to Congress published in July 2022.
A Unified Post-Acute Care PPS could help move the Medicare program toward a more equitable provision of PAC by better aligning payments and financial incentives with patient need. This could, in turn, lead to greater efficiency and a reduction in Medicare expenditures for PAC by streamlining payment policy for PAC and by basing payment on patient need regardless of setting.

Read the Report to Congress (2022)
Report to Congress: Unified Payment for Medicare-Covered Post-Acute Care
Analysis and Development of the Prototype Unified PAC Prospective Payment System Called for in the IMPACT Act
Constructing a PAC PPS Prototype That is Both Unified AND Comprehensive
Reflecting the diverse range of Medicare beneficiaries who receive post-acute care and their unique needs, the Prototype Unified PAC PPS sets payment by assigning Medicare beneficiaries in a uniform manner to one of more than 4,400 distinct payment groups.
(See Graphic 1, The Prototype Unified PAC PPS Framework)
The post-acute care unified payment prototype assigns each patient to the appropriate payment group using the following framework:
- Unified PAC Clinical Groups (UPCG): 32 clinical condition groups represent the patient’s primary reason for PAC, organized into three overarching categories:
- Rehabilitation and Therapy-Focused (Rehabilitation)
- Medical and Diagnosis-Focused (Medical)
- Medication Management, Teaching, and Assessment (MMTA)
- PAC Case-Mix Groups (P-CMG): Subgroups within each of the 32 UPCGs based on patients’ clinical characteristics, including:
- Self-care and mobility (motor) function (as reported using standardized data elements on the PAC assessment instrument) at admission; higher scores indicate higher functional abilities
- Primary PAC diagnosis
- Diagnoses and procedures reported during a prior acute care stay
- Additional adjustments for beneficiary and provider characteristics, including:
- Comorbidity Groups: Sub-groups reflect the relative costliness of the combination of secondary diagnoses reported on the PAC claim and information reported on the PAC assessment instrument. Payment adjustment for these groups varies across UPCGs.
- PAC Setting Types: An adjustment accounts for the relative costliness of treating the patient in different settings, which also varies across UPCGs
- Rural Settings: An adjustment applied to post-acute care claims from rural providers, which may also vary across UPCGs
- Cost Outliers: A separate payment group for cost outliers to ensure that their needs are adequately addressed
Graphic 1: The Prototype Unified PAC PPS Framework
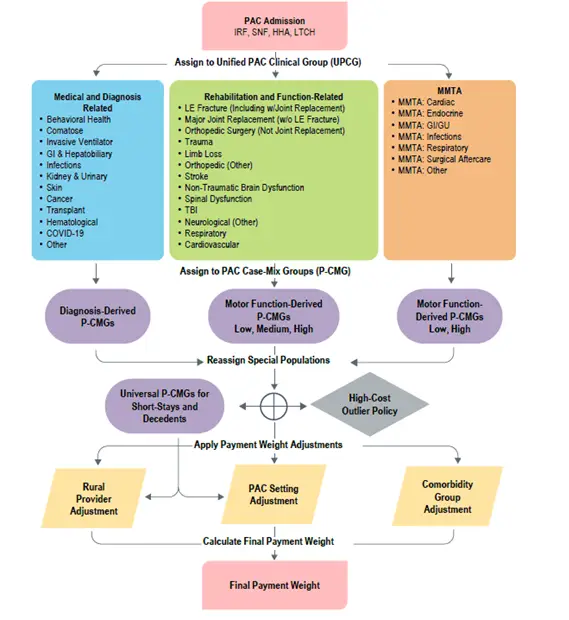
Notes:
GI = Gastrointestinal; GU = Genitourinary; LE = Lower Extremity; TBI = Traumatic Brain Injury.
“Decedents” refers to PAC stays where the beneficiary is recorded as having been discharged dead on the claim.
“Short stays” refers to IRF, SNF, and LTCH stays lasting no longer than 3 calendar days or HHA episodes lasting up to four visits and qualifying for Low-Utilization Payment Adjustment.
High-cost outliers were defined as having a claim cost more than three standard deviations from the mean within UPCG, P-CMG, and PAC provider type.
Unifying Post-Acute Care Payment: Recognizing That One Size Does Not Fit All
While the Unified PAC PPS is intended to standardize payment for similar patients across settings, stakeholders consistently noted that each of the four PAC provider types—IRF, SNF, HHA, and LTCH—provides unique services and tends to care for specific populations that sometimes overlap. The existing statutory payment systems were designed with these different services and populations in mind. A key consideration in developing the Unified PAC PPS was ensuring that this specificity was not lost when unifying payment policy across settings. The prototype was constructed in a way that incorporates key aspects of the current payment systems covering areas unique to their patient populations.
For example, the Home Health PPS contains clinical groupings for MMTA, which is a service primarily provided by HHAs in the context of PAC. Unlike in institutional PAC settings, under the current payment system patients with a cardiovascular diagnosis who are receiving home health are generally assumed to be receiving MMTA. We retained distinct MMTA groups for each of the relevant diagnoses from the Home Health PPS to ensure that this important service was properly captured. Similarly, clinical groups were included for patients who are comatose and who are on a ventilator upon admission to the PAC setting. Such patients are predominantly cared for in more intensive settings such as LTCH.
 We calibrated the prototype using Medicare PAC claims and assessment data from 2017 through 2020. Using these data, the model accounted for 48% of the variation in spending across the U.S., although some of this variation was attributable to the PAC setting. More importantly, payment weights generated by the prototype, on average, were consistent with actual estimated costs of care across PAC settings, clinical groups, geographic regions, and high- vs. low-cost PAC stays. Impacts to current payment amounts were modest across most of these groups.
We calibrated the prototype using Medicare PAC claims and assessment data from 2017 through 2020. Using these data, the model accounted for 48% of the variation in spending across the U.S., although some of this variation was attributable to the PAC setting. More importantly, payment weights generated by the prototype, on average, were consistent with actual estimated costs of care across PAC settings, clinical groups, geographic regions, and high- vs. low-cost PAC stays. Impacts to current payment amounts were modest across most of these groups.
What’s next for post-acute care payment systems?
While the prototype performed well across a wide range of PAC settings and patients, there are still several important considerations.
Long-term use of the setting adjustment
Although the goal of the Unified PAC PPS was to set payment based on patient characteristics, PAC setting continues to play an important role in determining payment under the prototype. The PAC setting adjustment was an important aspect of the prototype Unified PAC PPS because there are significant statutory and regulatory differences governing the different PAC settings (e.g., intensity of services). Differences such as these can have implications for costs of care above and beyond individual patient needs, and it was important to consider these differences to ensure equitable payment to providers, access to care for beneficiaries, and fair and reasonable payment for PAC across settings. However, in the long run, these PAC setting adjustments could also be modified should the regulations be changed as part of a broader effort to unify PAC policy.
COVID-19 and Payment System Changes in 2020
The COVID-19 pandemic and the public health emergency (PHE) wreaked havoc on the entire U.S. health care system. Post-acute care providers, in many ways, were hit especially hard. Additionally, new PAC payment frameworks were introduced to the Medicare benefit for HHAs and for SNFs in 2020. Unfortunately, limitations on data availability necessitated designing and calibrating the prototype using only data collected through 2020. Therefore, a key next step will be updating these analyses and evaluating the prototype using data that reflect the current state of Medicare-covered PAC.
Incorporating the unified Medicare payment system prototype into PAC assessments
Calibrating the prototype required using existing data to approximate how things like clinical group assignment could potentially function. More specifically, the prototype assumes the inclusion of a dedicated data element on each of the PAC assessment instruments for assigning patients to the appropriate clinical group for payment purposes. Because this data element is not present on the PAC instruments, we complied existing data from several sources including diagnoses from the PAC claim, prior service use, and the clinical groupings from the current payment systems—an approach that would likely be impractical in any future testing or implementation. Future work should begin by introducing, testing, and refining this new data element to maximize its utility in any future implementation efforts.
Harmonizing with existing programs and policies including beneficiary cost-sharing rules, value-based purchasing, and interoperability initiatives
Each of the PAC-setting-specific payment systems is complimented by an array of other setting-specific programs and policies including cost-sharing rules and value-based purchasing (VBP) initiatives. Each of these works in conjunction with the existing payment framework. Therefore, transitioning to a uniform payment framework would also require standardizing Medicare’s approach to these important policies. However, this does not necessarily require that all PAC settings be subject to the same cost-sharing rules or measured in the same manner for the purposes of VBP. For example, Home Health, which is typically the least-costly and most commonly used form of PAC, is not subject to cost-sharing. It may be beneficial in terms of costs to Medicare and beneficiary access, to maintain this incentive under the Unified PAC PPS.
Recognizing the impact of IT infrastructure on acute and post-acute care settings
Similarly, in recent years there has been a significant focus on enhancing the IT infrastructure in acute and PAC settings. A key element of this effort has been to facilitate appropriate information sharing across settings, as well as with patients, CMS, and other payers. One interoperability initiative, known as the Post-Acute Care Interoperability Workgroup (PACIO), aims to gain industry adoption by establishing a framework for the development of implementation guides and reference materials that will facilitate health data exchange through standards-based application programming interfaces. Broad-based adoption of information-sharing such as this could facilitate better communication and coordination across acute and PAC providers and could also be incorporated into a Unified PAC PPS or VBP initiative.
Ensuring post-acute care patients and providers aren’t left behind
An equitable approach to paying for PAC across settings must ensure that the needs of all patients are taken into account. Careful attention should be paid to how the prototype predicts patient needs and costs of care among vulnerable populations and patient groups who are cared for less frequently (i.e., not well represented in the data used to calibrate the payment system). Likewise, PAC providers span a range of specialties and facility types, and it will be important to ensure that those that treat less common clinical conditions or higher-need patients can continue needed services as the unified framework is further studied and tested.
Learn more about RTI’s work supporting value-based purchasing initiatives.
- Centers for Medicare & Medicaid Services (CMS)
- Office of the Assistant Secretary for Planning and Evaluation



