Better Cancer Care Through Aligned Financial Incentives and Improved Quality of Care
Objective
Provide higher quality, more highly coordinated care at the same or lower cost for Medicare beneficiaries receiving chemotherapy for cancer.
Approach
RTI is working with the Centers for Medicare & Medicaid Services (CMS) to monitor and implement the Oncology Care Model, an episode-based payment model that financially incentivizes high-quality, better-coordinated cancer care through two forms of payment to participating practices: monthly enhanced oncology service (MEOS) payments and the potential for performance-based payments based on high quality, lower cost care.
Impact
Guidance through the Oncology Care Model has led to a shift towards episode-based payment models for other cancer treatment modalities, including CMS’s forthcoming Radiation Oncology Model, set to launch January 1, 2022.
The Real Cost of Treating Cancer in the U.S.
Cancer is one of the most common and devastating diseases in the United States: more than 1.6 million people are diagnosed with cancer each year in this country. A significant proportion of those diagnosed with cancer are over 65 years old and are Medicare beneficiaries. Each year, cancer is responsible for the death of an estimated 600,000 Americans. The cost of cancer care reached at least $158 billion in 2020—an increase of 27% since 2010. The high cost of cancer treatment has left many patients and their families devastated by the expense, prompting a shift toward a value-based care system.
The Oncology Care Model: Value-Based Care for Better Treatment and Lower Costs
The Centers for Medicare & Medicaid Services’ (CMS) Innovation Center is furthering its goals of improved quality of care at the same or lower cost through an innovative oncology payment model, the Oncology Care Model (OCM). OCM is part of the larger U.S. health care movement towards paying providers based on the quality, rather than the quantity of care they give patients. The Oncology Care Model aims to ensure appropriate, high quality clinical cancer care throughout chemotherapy treatment sessions while reducing costs and improving health.
OCM is a 6-year value-based care model that began on July 1, 2016 and runs through June 30, 2022. OCM was CMS’s first value-based, episode-based specialty care payment model. Under OCM, physician group practices have entered payment arrangements that include financial and performance accountability for 6-month episodes of chemotherapy for Medicare beneficiaries with cancer. The Oncology Care Model currently includes:
- Approximately 130 participating chemotherapy centers that cover urban, suburban, and rural areas (See Figure 1)
- Practices that range in size from solo oncologists to large practices with hundreds of providers
- Chemotherapy centers participating in the OCM that are held accountable to:
- Provide enhanced patient navigation and care coordination services
- Increase patient access to providers 24 hours a day, 7 days a week
- Have conversations with their patients about the expected total cost of care for their cancer treatment
- Document that they provide cancer treatment that meets nationally recognized clinical guidelines
- Use data to drive continuous quality improvement.
Figure 1: Geographic Diversity of Participating OCM Cancer Centers

Value-Based Care in Action: Aligning Financial Incentives with Improved Quality of Care
OCM promotes whole practice transformation by incorporating a two-part payment system.
Regular monthly payment - A per-beneficiary Monthly Enhanced Oncology Services (MEOS) payment is made to the participating practice for any Medicare beneficiary with cancer who is receiving chemotherapy at the practice.
How It Works
- This payment occurs monthly for the duration of the episode, for a maximum of 6 months.
- The $160 per beneficiary per month MEOS payment assists participating practices in effectively coordinating and enhancing beneficiary care during chemotherapy treatment.
Performance-based payment - Participating practices have the potential for a performance-based payment, which incentivizes practices to lower the total cost of care and improve care for beneficiaries during treatment episodes.
Performance-based payments are made based on
- Practices’ episode costs being below target
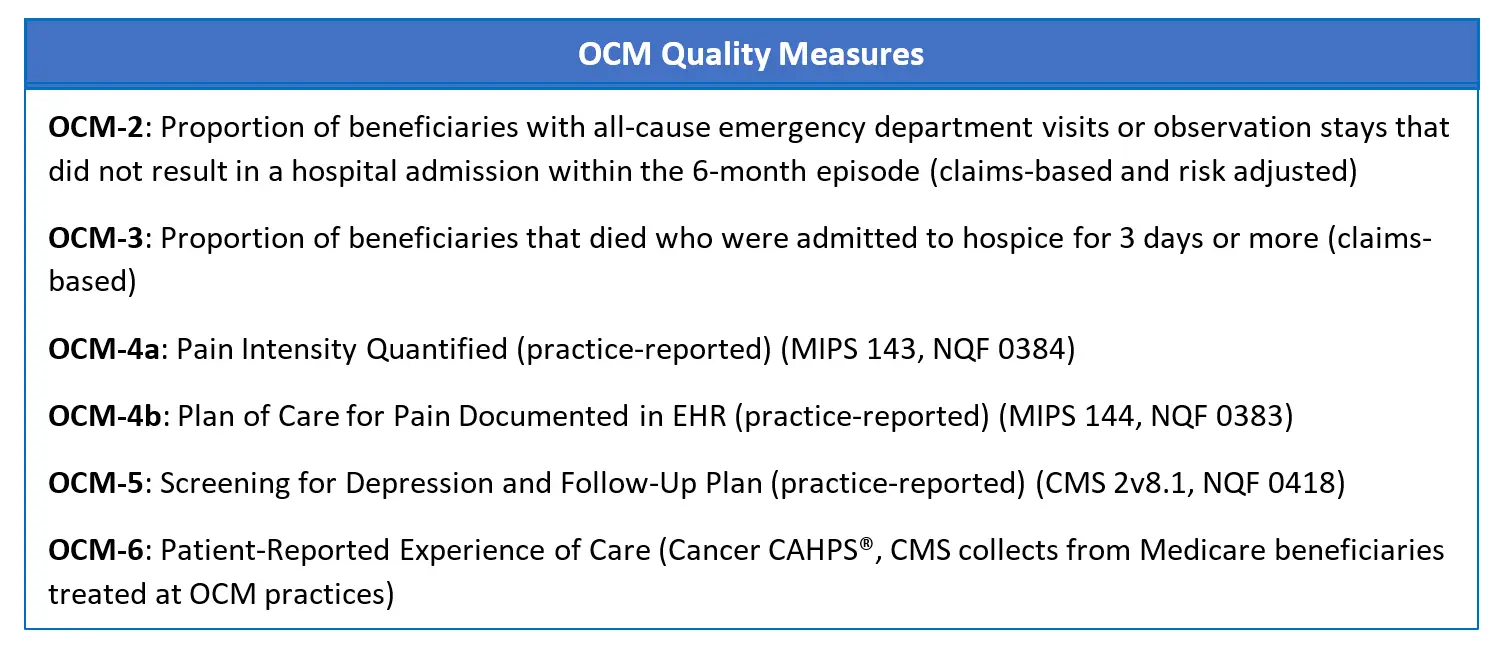
- Performance on quality measures (some claims-based, some practice-reported) that are measures of high quality, highly coordinated cancer care
RTI’s Contribution to OCM Implementation
RTI’s elite team employs a wide variety of skills and subject matter expertise: data analytics, financing, and quality of care measurement. RTI researchers are implementing and monitoring the OCM for CMS.
Oncology Care Model Implementation activities include:
- Beneficiary attribution
- Technical support to participating practices
- Quality measure specifications and calculations
- Quarterly practice feedback reports to practices
- Episode reconciliation
- Performance-based payment calculations
Oncology Care Model Monitoring efforts include:
- Site visits to assess practice transformation efforts
- Reviewing practices’ electronic health records (EHRs) to audit and validate practice-reported quality and clinical data
- Claims-based monitoring activities to examine aberrant practice patterns, altered patterns of treatment, or other unintended consequences of Model implementation
This OCM implementation work showcases RTI’s ability to provide insights and guidance at the forefront of clinical care in oncology. As the U.S. health system starts to shift towards value over volume, the OCM model of care and payment, and the forthcoming Radiation Oncology Model set to launch in 2022, will serve as examples of how the health care industry could shift its thinking and its practice towards high value, higher quality oncology care.
- Centers for Medicare & Medicaid Services (CMS)






