“Both my son and I have been victimized by this broken [addiction treatment] system. I have entrusted professionals with my son’s health and have rarely felt that he received effective care. It seems to be a business fraught with greed, false hope and ridiculous fees that play on parents' worst fears and anxiety.”
As this quote from the Partnership for Drug-Free Kids Parent Blog illustrates, the stakes of not providing addiction treatment quality measures are high, so I am pleased that the 2018 opioid bill, called the SUPPORT (Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment) for Patients and Communities Act, includes two new policies related to measuring the quality of opioid use disorder (OUD) treatment. We need this bill to begin to help patients and their families find quality, reputable addiction treatment.
The experience described above is, unfortunately, all too common. Individuals and family members searching for treatment have few ways to identify providers that are delivering effective treatment. According to the Substance Abuse and Mental Health Services Administration’s (SAMHSA’s) National Survey on Drug Use and Health, 20% of adults with unmet need for substance use disorder (SUD) treatment said they did not get treatment because they did not know where to go for care.
Individuals and their families who scan the Internet to find services—one of the most common ways to identify treatment providers—are confronted by an array of providers claiming to offer high-quality care. Online provider directories that purport to link patients with providers are sometimes driven by patient brokering schemes that refer patients to providers for a fee—without any effort to determine the most appropriate form of treatment.
Payers and health plans trying to contract with the best providers for their beneficiaries are faced with a similar lack of credible information on provider quality. The sad irony is that addiction treatment can be highly effective. Medications, such as methadone and buprenorphine, have been shown in numerous, large randomized clinical trials to significantly reduce the chance of dying and to significantly increase a person’s chance of being able to function in major life domains, such as work and family. Unfortunately, most addiction programs are not providing effective treatment. Less than half of addiction treatment programs, for example, can prescribe any of the medications approved by the Food and Drug Administration to treat opioid or alcohol use disorders.
The SUPPORT bill includes a requirement for the U.S. Department of Health and Human Services to start measuring the quality of opioid addiction treatment and that the State Opioid Response (SOR) Grants—which provides states with almost $1 billion to expand access to OUD prevention and treatment access—include funding to develop the necessary infrastructure to measure treatment quality.
Together, these initiatives can help to start to develop credible information that patients, families, payers can use to select high-quality treatment. However, those of us who have spent years developing and implementing quality in health care know that developing good quality measures is complex, so the adage of “what gets measured gets done” needs the following footnotes:
- If the measures are meaningful, reliable, and valid
- If the data do not require hours of data collection from overtaxed providers
- If the measures are actionable and providers have the means to improve the measure
I see these challenges play out daily through my work with government agencies and other clients who use data to measure and improve the response to the opioid crisis. And although the challenges are not insurmountable, they require careful planning, expertise, multistakeholder collaboration, and ongoing evaluation
In our work to develop actionable and meaningful quality measures for opioid treatment, we are following a rigorous process, which is outlined below.
From the RTI Press
Tracking the quality of addiction treatment over time and across states
This study analyzed the National Survey of Substance Abuse Treatment Services from 2007 through 2017 to determine the percent of facilities having the characteristics of higher quality.
What Do You Measure?
The first challenge is figuring out what to measure. There are hundreds of measures used across Federal and state governments. (For example, see the expansive list of measures used by the Centers for Medicare & Medicare Service and the measurement requirements for SAMHSA’s SOR grantees.)
As part of RTI International’s work with several states, we have developed summaries of the various measures that characterize their relative importance for improving addiction treatment outcomes, their validity and reliability, and whether providers know to implement changes to improve the quality of their treatment.
Will Providers Measure It?
Addiction treatment providers are typically overloaded with data collection requirements stemming from public funding agencies. However, we have found that if providers realize that the measures will be a tool to help them serve their clients more effectively and efficiently, the time spent collecting measures is viewed as a value-add. As a result, after we have identified a preliminary list of measures, we then obtain feedback from providers on whether the measures are meaningful, actionable, and not too burdensome to collect.
How Do You Create the Measures?
Quality measures can be created using a variety of data sources, including insurance claims, provider surveys, patient assessments, patient surveys, and electronic health data. Our focus in helping our clients is to minimize the burden of creating quality measures, while still ensuring that the quality measures capture important information and are useful. We are able to do this because we know the data resources that states already have, including data specific to behavioral health providers; we understand how states can leverage existing measures and reporting requirements to create new measures; and we are steeped in the nitty gritty details of measurement using claims data, surveys, and existing patient assessments.
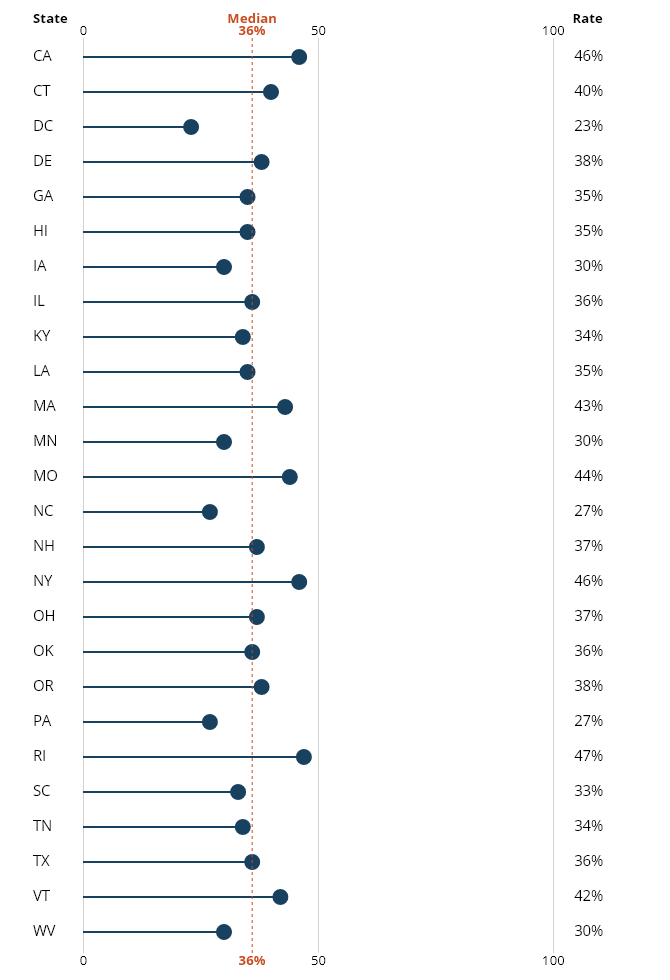
Once the measure is implemented, the work does not stop. Organizations need to know how to improve their treatment quality and have the motivation to do so. Take, for example, the Initiation and Engagement measure that has been reported by Medicaid-managed care plans for over 10 years. The Initiation measure captures whether people diagnosed with a SUD received treatment within 14 days. The Engagement measure captures whether those people stayed in treatment for a 30-day period. Rigorous research has shown that people with SUDs who meet the Initiation and Engagement criteria are less likely to die than those who drop out of treatment before hitting these benchmarks. However, initiation and engagement rates have not improved, suggesting organizations have not been given the means or motivation needed. In 2016, all Medicaid programs reported that less than 50% of patients stayed in treatment more than 14 days after their initial diagnosis.The chart below shows each state’s performance on the “Initiation and Engagement of Alcohol and Other Drug Dependence Treatment.”
Avoid the Pitfalls of Quality Measurement
Quality measures are powerful catalysts for quality improvement. Realizing their potential means avoiding these common challenges:
- Investing too little time and analysis in measure selection
- Selecting too many measures
- Failing to vet the measures with providers
- Garnering too few resources to efficiently create and disseminate the measures
- Neglecting to give guidance to providers on how to improve the measures
Measurement is a Critical Foundation to Reducing the Impact of the Opioid Epidemic
Quality measurement has been shown to be a powerful tool for saving lives and improving the quality of life. CMS’s 2018 National Impact Assessment Quality Measures Report described the following fantastic improvements as a result of their quality measures:
- 670,000 additional patients with controlled blood pressure (2006–2015)
- 510,000 fewer patients with poor diabetes control (2006–2015)
- 12,000 fewer deaths following hospitalization for a heart attack (2008–2015)
- 70,000 fewer unplanned readmissions (2011–2015)
- 840,000 fewer pressure ulcers among nursing home residents (2011–2015)
- 9 million more patients reporting a highly favorable experience with their hospital (2008–2015)
Imagine if in a few years we could report similar statistics for OUDs:
- Thousands of patients with OUD systems successfully managed on a combination of medication and therapy
- Thousands of fewer patients dying from opioid-related overdoses
- Thousands of fewer patients being admitted to the hospital and emergency department for opioid overdose deaths
- Thousands more patients successfully initiating and engaging in treatment.
With billions of dollars being dedicated to addressing OUDs, now is the time for states to develop a robust quality measurement foundation to guide and ensure progress in reducing the impact of this deadly disease.
