Evaluating the Accountable Health Communities Model to test whether connecting people to community resources to address health-related social needs can improve health outcomes and reduce costs
The economic and social conditions in which people are born, grow, work, live, and age are increasingly recognized as important drivers of their health and well-being. These conditions, known as social determinants of health (SDoH), are just as important—if not more so—as clinical care for determining health outcomes. Adverse impacts of SDoH fall disproportionately on racial and ethnic minorities, low-income populations, individuals with limited English proficiency, people with disabilities, and other groups. The COVID-19 pandemic is a stark reminder about the consequences of SDoH for the burdens of illness and death.
Addressing Social Determinants of Health
Addressing SDoH is central to reducing health disparities and increasing health equity. Strategies for addressing SDoH can target underlying community-level social and economic conditions or individual-level health-related social needs (HRSNs), such as food insecurity and housing instability. For both community-level and individual-level strategies, data are critical to
- Documenting health disparities associated with SDoH
- Identifying individuals and communities that can benefit most from addressing the adverse impacts of SDoH
- Designing effective policies and interventions
- Measuring whether the policies and interventions increase health equity and reduce disparities.
However, the data needed for those strategies, including data to identify and document SDoH, are often lacking. The Accountable Health Communities (AHC) Model is a major Centers for Medicare & Medicaid Services (CMS) initiative that aims to fill this gap. The AHC Model tests whether screening Medicare and Medicaid beneficiaries for HRSNs and using navigators to connect qualified beneficiaries to community resources to address their needs can improve health outcomes and reduce costs. (Qualified beneficiaries have an HRSN and at least two emergency department visits in the year before screening.)
Evaluating the Accountable Health Communities Model
As the evaluator of the AHC Model, RTI International analyzed rich data from model participants. These data provide information about (1) whether any of the five core HRSNs (i.e., food insecurity, housing instability, transportation problems, utility difficulties, and interpersonal violence) are prevalent among screened Medicare and Medicaid beneficiaries; (2) whether beneficiaries were successfully connected to community resources; and (3) whether their needs were resolved.
We utilized a mixed methods evaluation design to
- Understand how the AHC Model was implemented
- Assess success in connecting beneficiaries to community resources and resolving their HRSNs
- Measure impacts on health care utilization and expenditures
- Understand how implementation and contextual factors are associated with model impacts.
The evaluation draws on various data types and sources—including model participant data, publicly available data to describe community context, fee-for-service claims and Medicare Advantage encounters for Medicare beneficiaries, Transformed Medicaid Statistical Information System (T-MSIS) data for Medicaid beneficiaries, key informant interviews, and beneficiary and organizational surveys. To evaluate health care utilization and expenditure impacts, we took advantage of random assignment of beneficiaries to the model intervention in some areas; in other areas, we utilized quasi-experimental difference-in-differences analysis.
Understanding the Findings
The second evaluation report presents our findings that the AHC Model led to a reduction in emergency department visits for both Medicaid and fee-for-service Medicare beneficiaries. Interviews with AHC Model stakeholders revealed a positive impact on their engagement with the healthcare system. By fostering trust navigators were able to effectively empower beneficiaries to be more proactive in seeking suitable care, which potentially decreased emergency department visits. This finding underscores the importance of personalized assistance and highlights the potential of navigation services in bridging the gap between healthcare services and individuals facing social determinants of health.
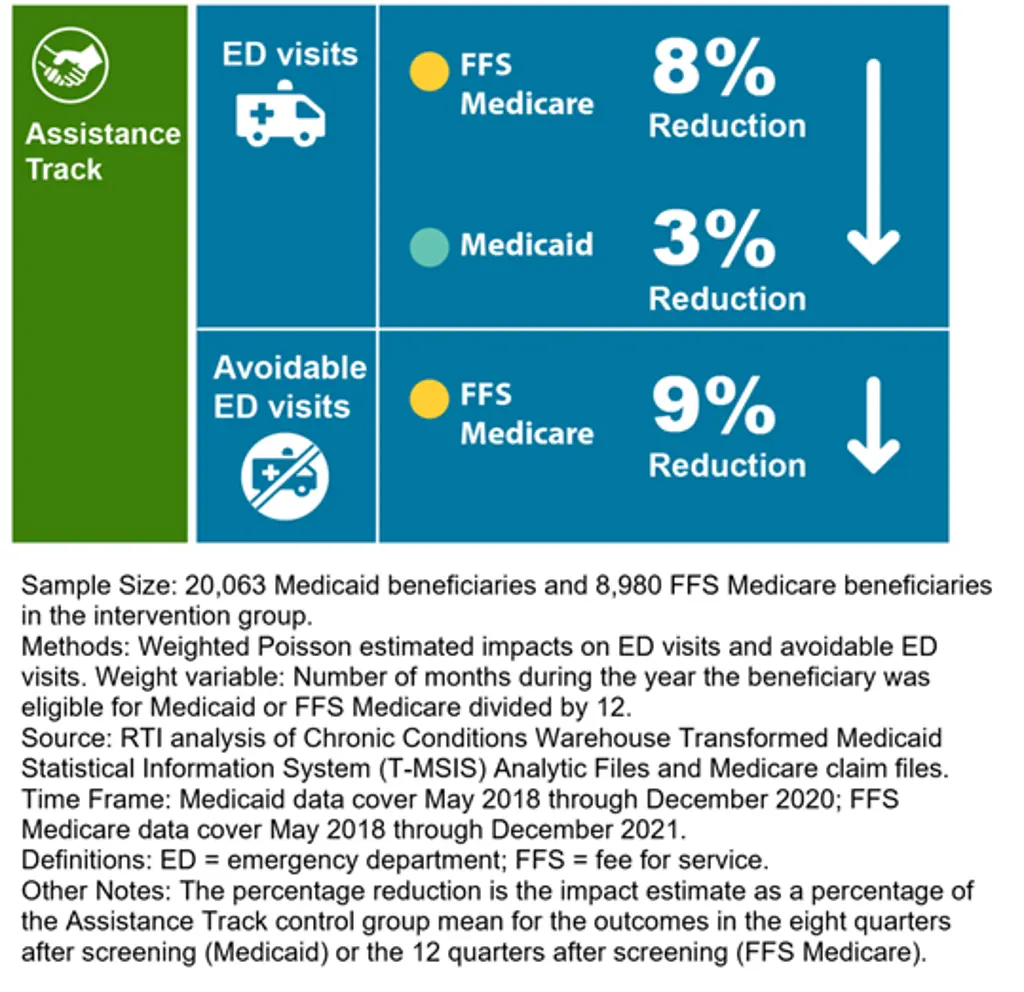
Assistance Track Impacts on Emergency Department Visits
The study's findings provide mixed evidence regarding the impact of engaging beneficiaries with health-related social needs on other healthcare outcomes. Nonetheless, the significant reduction in emergency department visits and stakeholder testimonies demonstrate the potential of the AHC Model in improving healthcare delivery. As efforts to address social determinants of health continue, the model serves as a vital initiative, emphasizing the importance of a comprehensive approach that recognizes and tackles the social factors impacting individual well-being.
Moving Forward: Using Data to Reduce Disparities
The Accountable Health Communities Model has shown promise in addressing social determinants of health and enhancing healthcare outcomes. The reduction in emergency department visits signifies its positive impact on patient outcomes and resource allocation. As the healthcare landscape evolves, the AHC Model serves as a prototype for change, inspiring a patient-centered and holistic approach that addresses the social factors influencing health.
Learn More
For more about this project, read the complete Accountable Health Communities (AHC) Model Evaluation: Second Evaluation Report.
- Center for Medicare and Medicaid Innovation (CMMI)
- Abt Associates
- Social Interventions Research & Evaluation Network (SIREN) at the University of California San Francisco
- Inciter




